Objectives. Gestational diabetes is a frequent complication in recent years associated with excessive weight or obesity. On the other hand, gestational hypertension is an independent entity in pregnancy or possible associated with gestational diabetes and obesity. Implication. Few cases of gestational diabetes associate hypertension or fetal distress. Material and methods. In the cases born in “Alfred Rusescu” Institute for Mother and Child Care/Polizu, Neonatology Clinic, Bucharest, in 2015, mothers who developed gestational diabetes have experienced other complications (stained amniotic fluid, thrombophilia, arterial hipertesion, cholestasis). In one case, preexisting hypertension pregnancy was associated with gestational diabetes, resulting a term neonate, large for gestational age, extracted by caesarean in cranial presentation. Results. Gestational diabetes influenced fetal antopometric indicators and not hypertension. Conclusions. The association of gestational diabetes, maternal obesity and hypertension in pregnancy requires further investigation, fetal monitoring and perinatal team for an uncomplicated adaptation of the newborn to life outside the womb. Originality value. Maternal pregnancy hypertension affects fetal nutrition and the result is intrauterine growth restriction, iatrogenic prematurity and fetal distress. Gestational diabetes with hypertension has an influence on antopometric indicators, giving birth to infants with higher weight for gestational age.
Diabetul şi hipertensiunea arterială gestaţională - impactul asupra nou-născuţilor
Gestational diabetes and hypertension - outcome of newborns
First published: 15 aprilie 2016
Editorial Group: MEDICHUB MEDIA
Abstract
Rezumat
Obiectiv. Diabetul gestaţional este o complicaţie frecventă în ultimii ani, asociată cu greutate excesivă sau obezitate. Pe de altă parte, hipertensiunea gestaţională este o entitate independentă în timpul sarcinii sau posibil asociată cu diabetul gestaţional şi obezitatea. Impact. Câteva cazuri de diabet zaharat gestaţional asociază hipertensiune de sarcină sau suferinţă fetală. Material şi metodă. În cazurile de copii născuţi în Institutul pentru Sănătatea Mamei şi Copilului „Alessandrescu-Rusescu”/Polizu, Clinica de Neonatologie, Bucureşti, în 2015, mamele care au dezvoltat diabet gestaţional au avut şi alte complicaţii (lichid amniotic meconial, trombofilie, hipertesiune arterială, colestază). Într-un caz de hipertensiune preexistentă sarcinii a fost asociat diabet gestaţional, având ca rezultat un nou-născut la termen, mare pentru vârsta gestaţională, extras prin operaţie cezariană din prezentaţie craniană. Rezultate. Diabetul gestaţional a influenţat indicatorii antropometrici fetali, şi nu hipertensiunea. Concluzii. Asocierea diabetului gestaţional, obezitatea maternă şi hipertensiunea arterială în timpul sarcinii necesită investigaţii suplimentare, monitorizare fetală şi echipă perinatală pentru o adaptare necomplicată a nou-născutului la viaţa extrauterină. Originalitate. Hipertensiunea de sarcină afectează nutriţia fetală, iar rezultatul este restricţia de creştere intrauterină, prematuritate şi suferinţă fetală. Diabetul gestaţional cu hipertensiune are o influenţă asupra indicatorilor antopometrici care dau naştere la copii cu greutate mai mare pentru vârsta gestaţională.
Introduction
It is well known that, during its clinical course, diabetes mellitus may be accompanied by several other morbid conditions and may be labeled as “co-morbidities”. However, a clear delimitation between these two categories is not always possible; for some entities we do not have decisive arguments to include them in one or another category(1).Co-morbidities that are worth being commented regarding their genetic background are the following: obesity, dyslipidemia, arterial hypertension and metabolic syndrome(1).
Most women who have gestational diabetes deliver healthy babies. However, gestational diabetes that’s not carefully managed can lead to uncontrolled blood sugar levels and cause problems for mother and newborn, including an increased likelihood of needing a C-section to deliver. It is more likely to develope once again gestational diabetes during a future pregnancy and to develop type 2 diabetes in time. Out of those women with a history of gestational diabetes who reach their ideal body weight after delivery, fewer than 1 in 4 eventually develops type 2 diabetes(2).

Diabetes mellitus and obesity
Recent studies have demonstrated that the repartition of adipose tissue has a major influence on the risk of obesity-related conditions development. The abdominal storage of the adipose tissue (with its two components: visceral and subcutaneous), known as central obesity, is correlated with a higher risk for cardiovascular diseases, arterial hypertension and metabolic disorders, insulin resistance and endothelial dysfunction(1).
It was studied the incidence of gestational diabetes mellitus (GDM) in relation to phenotypic characteristics and gestational weight gain (GWG) among women at high risk for GDM(3). There was no interaction between GWG and GDM outcome and no significant difference in the prevalence of diabetes-associated antibodies. GWG and the presence of diabetes-associated antibodies were not associated with GDM occurrence among these high-risk women. Despite a healthier metabolic profile at baseline, the non-obese women with previous gestational diabetes mellitus display a markedly higher cumulative incidence of gestational diabetes mellitus(3).
The discovery of genes (also known as quantitative trait loci - QTLs) contributing to blood pressure control is considered an important tool in elucidating the pathogenic mechanisms that lay behind essential hypertension(1).
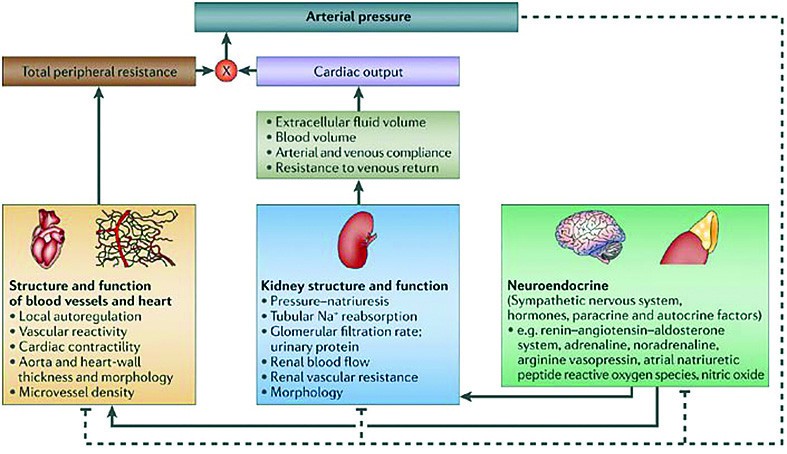


Diabetes mellitus and blood pressure
A genome-wide scan (GWS) for the discovery of BP genes can be described as a search for QTLs across the entire genome using anonymous, highly polymorphic (and thus genetically informative) microsatellite (MS) markers in large cohorts of families with hypertension traits. As a result, more than 100 hypertension gene variants (QTLs) were described, with at least one hypertension QTL on each chromosome(1).
It can be expected that in the following years, due to the quick advances in genotyping technology and computing methods, better designed and enlarged GWA scans will provide novel, unbiased information about the heritable basis of hypertension at a level of detail that has not been possible previously(1).
Gestational diabetes and pregnancy-induced hypertension are common, and their relation is not well understood(4).
Hypertensive disorders of pregnancy complicate 5-10% of all pregnancies and can result in a variety of maternal and fetal complications, including seizures, stroke, hepatic failure, renal failure, intrauterine growth retardation, fetal distress, premature delivery, and death(4).
Like pregnancy-induced hypertension, gestational diabetes mellitus is also relatively common and affects 3-5% of pregnancies, resulting in a variety of complications that primarily affect the fetus, including macrosomia, stillbirth, jaundice, and respiratory distress syndrome(4).
In this large, population-based study, we found a significantly increased risk of gestational hypertension, mild pre-eclampsia, and severe preeclampsia among women with gestational diabetes. The risk for pregnancy-induced hypertension associated with gestational diabetes varied among different maternal ethnicity groups and also by degree of prenatal care(4).
There is little direct clinical evidence on the reverse issue, but data are presented to suggest that pregnancy-induced hypertension may only predispose to gestational diabetes when its etiology is gestational hypertension and not preeclampsia(5).
Preeclampsia and gestational diabetes also affected the newborns. Women with preeclampsia were more likely to give birth to underweight babies and deliver prematurely. Women with gestational diabetes were more likely to deliver overweight babies(6).
Experimental
The study from Polizu Maternity analyzed pregnant women with gestational diabetes and their newborns. One case was of type 1 diabetes mellitus.Newborns of women with gestational diabetes type 2 were macrosoms, developing early neonatal pathology, metabolic (hypoglycaemia and/or hypocalcemia), plastic lesions (fetal borderline position determined by fetal-uterus disproportion), and injuries induced by the act of birth due to neonatal antopometric measurements located on the 90th percentile for gestational age and over.
There were minor injuries type facial bruising, caput succedaneum, cephalhematoma, despite the fact that over 80% of fetuses were extracted by caesarean section.
Please note that the indication for caesarean section was in 60% of cases the scar in the uterus, and the newborns were large for gestational age, that could induce maternal and fetal/neonatal morbidity during labor.
It was not registered changes in blood pressure, heart rate or another cardio-circulatory pathology in these newborns.
In type 1 diabetes, cardiac structural modification was registered by patent ductus arteriosus.
Results
Gestational diabetes influenced fetal antopometric indicators and hypoglycemia as metabolic disorder and not hypertension.Discussion
Maternal pregnancy hypertension affects fetal nutrition and the result is intrauterine growth restriction, iatrogenic prematurity and fetal distress. Gestational diabetes with hypertension has an influence on antopometric indicators, giving birth to infants with higher weight for gestational age.Conclusions
The association of gestational diabetes, maternal obesity and hypertension in pregnancy requires further investigation, fetal monitoring and perinatal team for an uncomplicated adaptation of the newborn to life outside the womb.Bibliografie
2. Mayo Clinic, Diseases and Conditions, Gestational diabetes, Complications, available from http://www.mayoclinic.org/diseases-conditions/gestational-diabetes/basics/complications/con-20014854
3. Huvinen E et al., Heterogeneity of maternal characteristics and impact on gestational diabetes (GDM) risk-Implications for universal GDM screening?, Ann Med. 2016 Jan 8:1-7.
4. Chris L. Bryson et al., Association between Gestational Diabetes and Pregnancy-induced Hypertension, Oxford Journals Medicine & Health, American Journal of Epidemiology, Volume 158, Issue 12, Pp. 1148-1153.
5. Roberts R, Hypertension in women with gestational diabetes, Diabetes Care. 1998 Aug; 21 Suppl 2:B27-32.
6. Howard LeWine, Pregnancy-related high blood pressure, diabetes linked to later heart disease, available from Harvard Health Blog, http://www.health.harvard.edu/blog/pregnancy-related-high-blood-pressure-diabetes-linked-to-later-heart-disease-201202224309.
Articole din ediţiile anterioare
Restricţia de creştere intrauterină - o nouă abordare
Restricţia de creştere intrauterină este definită de imposibilitatea fătului de a-şi atinge potenţialul de creştere programat; în absenţa unui g...
Particularităţi ale evoluţiei materno-fetale la pacientele cu diabet gestaţional
Studiul elaborat a avut ca obiectiv identificarea complicaţiilor, a factorilor de risc şi a altor particularităţi asociate diabetului gestaţional.
Modificări metabolice şi structurale descoperite prin rezonanţă magnetică la feţii cu restricţie de creştere intrauterină
Restricţia de creştere intrauterină (RCIU) afectează 5-10% dintre sarcini şi include tulburări cognitive la copii într-o proporţie substanţială, as...
Diabetul gestaţional şi diabetul preexistent sarcinii – abordare din perspectiva metforminului
În diabetologie, metforminul este utilizat frecvent, existând o vastă experienţă în utilizarea sa, cu multiple beneficii şi costuri reduse. Din ce ...