Abdominal pregnancy is a very rare form of ectopic pregnancy and is associated with an increased mortality rate. The main life-threating complication is intraperitoneal bleeding from placental site. The gestational age is important for the prediction of complications’ severity. While most cases are secondary to a tubal rupture and the subsequently implantation in the peritoneal cavity, a previous uterine perforation can also represent the leading cause. In the current paper, we report an extremely rare case of secondary abdominal pregnancy with a gestational age of 11 weeks in a 37-year-old patient having a history of unnoticed uterine perforation. This report raises awareness on a rare and severe obstetrical condition, discussing the case particularities, with the aim to highlight the urge for prompt diagnostic and treatment measures.
Un caz rar de sarcină abdominală secundară – prezentare de caz şi review al literaturii
A rare case of secondary abdominal pregnancy – case report and literature review
First published: 24 martie 2022
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.35.1.2022.6125
Abstract
Rezumat
Sarcina abdominală este o formă foarte rară de sarcină extrauterină şi este asociată cu o rată ridicată a mortalităţii. Principala complicaţie ameninţătoare de viaţă este hemoperitoneul cu punct de plecare la nivelul inserţiei placentare. Vârsta gestaţională este importantă pentru predicţia severităţii complicaţiilor. În timp ce majoritatea cazurilor sunt consecinţa unei rupturi tubare cu implantare secundară în cavitatea peritoneală, istoricul unei perforaţii uterine poate reprezenta, de asemenea, o cauză de sarcină secundară abdominală. În această lucrare, raportăm un caz extrem de rar de sarcină abdominală secundară cu o vârstă gestaţională de 11 săptămâni la o pacientă de 37 de ani cu antecedente de perforaţie uterină care a rămas nediagnosticată. Scopul acestei lucrări este de a creşte gradul de conştientizare asupra unei afecţiuni obstetricale rare şi severe, discutând particularităţile cazului, cu scopul de a evidenţia necesitatea implementării prompte a măsurilor de diagnostic şi tratament corespunzătoare.
Introduction
Abdominal pregnancy (AP) represents around 1% of all ectopic pregnancies, with an incidence ranging between 1:10000 and 1:30000 pregnancies(1). It is the rarest type of ectopic pregnancy, but the only one that can result in the delivery of full-term baby, although most cases are earlier complicated by massive hemorrhage due to placental site detachment. The maternal mortality rate varies, among publications, between 0.5% and 18%, and the perinatal mortality is up to 80%(2).
Abdominal pregnancy is defined as a pregnancy developing within the peritoneal cavity, outside genital organs(3). Ordinarily, the location of an AP is in the pelvis, with the most common implantation site being the posterior cul-de-sac, followed by the mesosalpinx, omentum and uterine serosa(3). Very rarely cited localization of AP include retroperitoneal space(4), appendix(5), liver(6) or even thoracic cavity(7). The diagnosis of these unusual ectopic locations is frequently made at the time of the surgical intervention, but the possibility of bizarre clinical presentations for abdominal pregnancies should be kept in mind, since there are no pathognomonic symptoms of abdominal pregnancy.
Abdominal pregnancies can be classified as primary or secondary(8). Primary abdominal pregnancy occurs when the fertilized ovum implants directly into the peritoneal cavity(9). On the other hand, secondary abdominal pregnancy (the more common type) occurs when the fertilized ovum subsequently reaches the abdominal cavity after the primary implantation at any ectopic site, usually after a tubal rupture. Other causes of secondary AP include the rupture of a uterine horn or previous caesarean scar(10) and, extremely rare, an iatrogenic perforation of the uterus.
A high index of suspicion for this rare obstetrical event, along with continues professional development are required to establish the diagnosis of AP, but most cases require ultrasonography and magnetic resonance imaging for clinching the diagnosis, while the measurement of human chorionic gonadotropin is important for otherwise unexplained masses or intraperitoneal hemorrhage(11). Still, there is no evidence-based therapeutic strategy planned for AP so far in the literature.
Case report
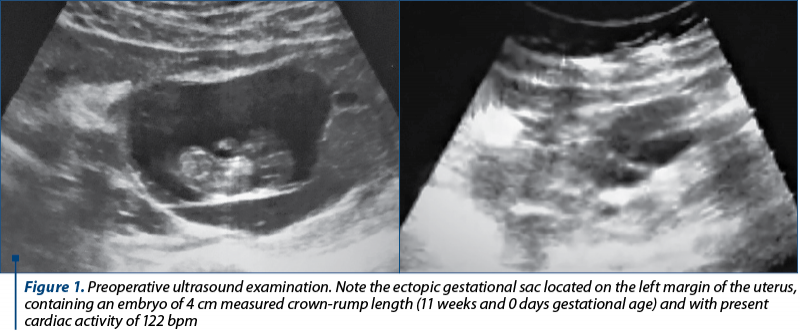
A 37-year-old woman (gravida 4, para 2) was referred to the Bucharest University Emergency Hospital with a suspicion of ruptured ectopic pregnancy. She had a history of two vaginal deliveries and two induced abortions, the last one occurring eight years ago. At the time of presentation, the patient affirmed two weeks of amenorrhea with irregular menstrual cycle within the last four months, despite taking combined oral contraceptive pills for the last eight years. She accused intense headache and acute postcoital pelvic pain, followed by lipothymia. At admission, the patient was lucid, but hemodynamically and respiratory instable, afebrile, presenting diffuse abdominal tenderness, guarding, rebound tenderness and no genital bleeding on pelvic examination. Ultrasonography demonstrated massive intraperitoneal bleeding and a gestational sac containing a live 11-week embryo, with the sac positioned outside the uterine cavity (Figure 1). The patient’s hemoglobin level and hematocrit were 9.4 g/dL and 25.5%, respectively. Emergency exploratory laparotomy was performed for hemoperitoneum and suspicion of abdominal pregnancy.
A vertical incision of the lower abdomen with the patient under general endotracheal anesthesia revealed around 2000 mL of hemoperitoneal fluid. The exploration of the abdominal cavity revealed normal bilateral adnexa, a small uterus and a gestational sac of about 7 cm diameter with integer amnion, partially covered by thin trophoblastic tissue (Figure 2) and large blood clots. Complex vascularization of the trophoblast appeared to come from epiploic vessels and abnormal tissue on the uterine fundus that presented active bleeding (Figure 3).

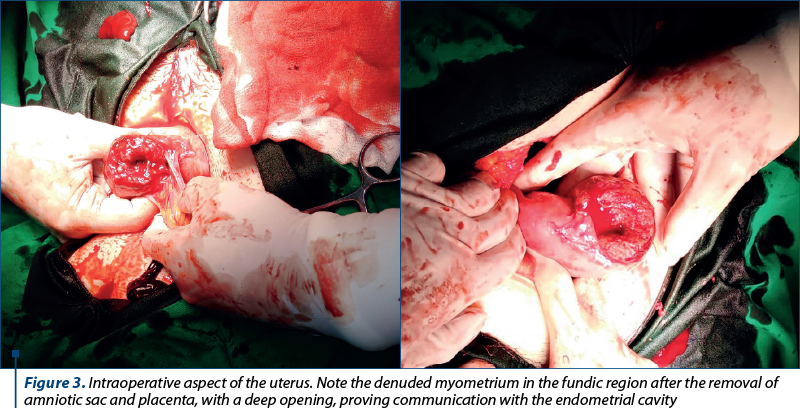
The resection of the trophoblastic implant from the uterus revealed a communication to the endometrial cavity (Figure 3), suggestive for secondary abdominal ectopic pregnancy following old iatrogenic uterine perforation.
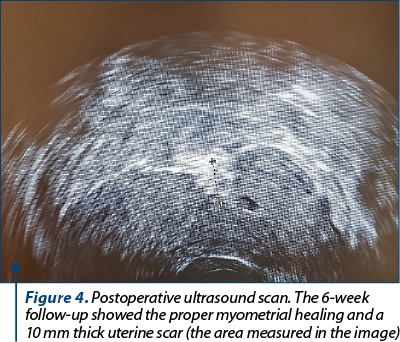
Partial omentectomy was performed, along with curettage of the uterine cavity through the opening resulted after uterine perforation, despite no macroscopic evidence of profound trophoblastic tissue. Two layers of interrupted sutures helped controlling the bleeding from the uterine denuded area. No other bleeding lesions were found, the abdominal cavity was washed with saline, and an abdominal drain was inserted. The patient received an intraoperative blood transfusion and one unit of fresh frozen plasma. The postoperative course proceeded uneventfully and the patient was discharged after four days with instructions for outpatient follow-up.
The histopathological examination of the excised tissue revealed the presence of trophoblastic and decidual tissues within blood clots and an embryo with no structural malformations. The follow-up scan revealed a favorable postoperative appearance of the myometrial defect area (Figure 4).
Discussion
In the last decades, the incidence of ectopic pregnancy has increased, while the case fatality rate has declined significantly, given the advance in diagnostic modalities, the prompt treatment measures and the availability of life-saving anesthesiology measures(12). Still, a large proportion of nontubal ectopic locations are diagnosed in the operating room or are never known due to a successful response to medical management for a pregnancy of unknown location. In this regard, raising awareness among medical specialists regarding the variable clinical presentation and the risk factors is still promoted.
Despite being a rare condition, abdominal pregnancy has a maternal mortality around eight times greater than other ectopic pregnancies(13), due to placental separation and to unpredictable even catastrophic intraabdominal bleeding. There is also a high risk of maternal coagulopathy, embolism, fistula formation and fetal malformations(14).
The most important factors that influence the clinical presentation, survival and management modality include maternal hemodynamic status and gestational age at the time of presentation(3). There is no pathognomonic symptom for AP(13), most cases presenting for unexplained, persistent abdominal pain. The symptoms of early abdominal pregnancy (gestational age under 20 weeks) are rather similar to those of tubal abortion or rupture, self-limited bleeding in the placental site being a common finding, while for advanced AP, bleeding is more commonly catastrophic(14). Near-term abdominal pregnancy can present persistent nausea, breathing shortness, painful or decreased fetal movement(15).
The surgical removal of the fetus and placenta is the most accepted management option for early AP, dead or malformed fetus or in case of dreadful maternal complications(2,16). Future fertility can usually be preserved since fallopian tubes and ovaries are not directly involved in most abdominal pregnancies.
Minimally invasive laparoscopic and ultrasonically guided procedures have emerged in the literature in the last decade for early pregnancy presentations, as well as preoperative methotrexate administration or preoperative selective embolization of placental insertion(17). Given the advances in neonatology and preterm infant survival, the expectant management can be considered for an advanced pregnancy without decompensation or fetal malformation, with informed consent, multidisciplinary approach and careful monitoring in the hospital, constantly weighing the risk of the sudden onset of life-threatening maternal hemorrhage versus neonatal death. In our case, despite the viability of the pregnancy, the maternal hemodynamically instability and the evidence of massive internal hemorrhage urged for surgery.
For some cases, it may be impossible to differentiate between primary and secondary AP. In 1942, Studdiford(18) published some criteria to diagnose a primary abdominal pregnancy, including: normal fallopian tubes with no evidence of trauma, the absence of any uteroperitoneal fistula, and the presence of a pregnancy related exclusively to the peritoneal surface and early enough to eliminate the possibility of secondary implantation after a primary nidation within the tube. For our reported case, the second criterion could not be met since the fundic uterine serosa presented trophoblast invasion and active bleeding source, also revealing a communication with the endometrial cavity, thus the intraoperative findings support the hypothesis of a rather secondary abdominal pregnancy.
The possibility of abdominal pregnancy must be a part of the differential diagnosis of ectopic pregnancy and the complete history must be obtained, gaining information regarding contraction methods and possible uterine perforation history, since similar cases of AP following variable period after curettage for pregnancy termination were previously reported(19,20). The diagnostic tools include serial human chorionic gonadotrophin titers with suboptimal increase, ultrasound and MRI evaluation. Useful ultrasound features to aid diagnostic of AP include depiction of gestational sac or pelvic mass separate from the uterus or localization of the placenta outside the confines of the uterine cavity(21).
Addressing the association between contraceptive pills use and ectopic pregnancy rates, a multicenter case-control study of women from Shanghai showed that the current use of oral contraceptive pills can protect against unwanted pregnancy, both intrauterine and ectopic, but it can quadruple the risk of ectopic pregnancy following contraceptive failure compared with the risk associated with the non-use of any contraceptives(22).
Conclusions
There is no established guidance regarding the diagnosis and ideal treatment for abdominal pregnancies. The complete medical history can orient towards a high index of suspicion. Most cases require individualized management based on the particular case characteristics and the availability of experienced specialists. Except the extremely rare cases of term abdominal pregnancies and successfully births, this obstetrical condition is usually managed as nonviable and life threatening, the timely surgical intervention being imperative to avert grievous consequences.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- Mengistu Z, Getachew A, Adefris M. Term abdominal pregnancy: A case report.
- J Med Case Rep. 2015;9:168.
- Rohilla M, Joshi B, Jain V, Neetimala, Gainder S. Advanced abdominal pregnancy: a search for consensus. Review of literature along with case report. Arch Gynecol Obstet. 2018;298(1):1-8.
- Agarwal N, Odejinmi F. Early abdominal ectopic pregnancy: challenges, update and review of current management. Obstet Gynaecol. 2014;16(3):193-8.
- Hou Q, Xin L, Jian L, Pan J, Chen L, Song W. Retroperitoneal ectopic pregnancy: A case report and literature review. J Obstet Gynaecol Res. 2021;47(3):1186-90.
- Thompson RJ, Hawe MJG. A rare pathological trinity: An appendiceal ectopic pregnancy, acute appendicitis and a carcinoid tumour. Ir J Med Sci. 2011;180(2):579-80.
- Kuai XP, Wang SY, Qiu JM. Ectopic pregnancy implanted in the liver under the diaphragm. Taiwan J Obstet Gynecol. 2013;52(4):586-7.
- Fishman DA, Padilla LA, Joob A, Lurain JR. Ectopic pregnancy causing hemothorax managed by thoracoscopy and actinomycin D. Obstet Gynecol. 1998;91(5 Pt 2):837-8.
- Martin JN, McCaul IV JF. Emergent management of abdominal pregnancy. In: Clinical Obstetrics and Gynecology. 1990;33(3):438-47.
- Cîrstoiu M, Secară D, Secară I, Tufan C, Bohâlţea R. The relation between uterine scar determined by hysteroscopic procedures and acute abdomen during pregnancy - case series. Ginecologia.ro. 2015;8(2):6–11.
- Mittal SK, Singh N, Verma AK, Agarwal H, Kulkarni CD, Kanaujia R. Fetal MRI in the pre-operative diagnosis and assessment of secondary abdominal pregnancy: A rare sequela of a previous caesarean section. Diag Interv Radiol. 2012;18(5):496-502.
- Mai H, Dong T, Guo M, Mao Y, Peng X, Song T. MRI diagnosis of abdominal pregnancy. Chinese J Med Imaging Technol. 2018;12:386-90.
- Ben-Nagi J, Jurkovic D. Deaths in early pregnancy. The eight report of the confidential enquiries into maternal deaths in the United Kingdom. BJOG. 2011;118(11):1401-2.
- Poole A, Haas D, Magann EF. Early abdominal ectopic pregnancies: A systematic review of the literature. Gynecol Obstet Invest. 2012;74(4):249-60.
- Kunwar S, Khan T, Srivastava K. Abdominal pregnancy: Methods of hemorrhage control. Intractable Rare Dis Res. 2015;4(2):105-7.
- Hulsart-Billström G, Bergman K, Andersson B, Hilborn J, Larsson S, Jonsson KB. A uni-cortical femoral defect model in the rat: Evaluation using injectable hyaluronan hydrogel as a carrier for bone morphogenetic protein-2. J Tissue Eng Regen Med. 2015;9(7):799-807.
- Meng Q, Meng Q, Yu H, Wei X. A survey on sEMG control strategies of wearable hand exoskeleton for rehabilitation. 2017 2nd Asia-Pacific Conf Intell Robot Syst ACIRS 2017. 2017;165–9.
- Chan W, Shivji A, Murji A. Laparoscopic Management of an Abdominal Ectopic Pregnancy. J Minim Invasive Gynecol. 2021;28(11, Suppl.):S57.
- Studdiford WE. Primary peritoneal pregnancy. Am J Obstet Gynecol. 1942;44:487-91.
- Hernández Núñez J, Abreu Díaz A, Michael Ndwambi N, Luis Martínez F. Ectopic abdominal pregnancy due to uterine perforation after an attempt to terminate pregnancy: a case presentation. Medwave. 2017;7(6):e7000.
- Tubid R. Secondary abdominal pregnancy following uterine perforation.
- J Obstet Gynecol India. 2011; 61(4):443–4.
- Allibone GW, Fagan CJ, Porter SC. The sonographic features of intra‐abdominal pregnancy. J Clin Ultrasound. 1981;9(7):383-7.
- Li C, Zhao WH, Meng CX, Ping H, Qin GJ, Cao SJ, et al. Contraceptive use and the risk of ectopic pregnancy: A multi-center case-control study. PLoS One. 2014;9(12):e115031.
Articole din ediţiile anterioare
Receptorul şi rolurile gonadotropinei corionice umane în sarcină
Reproducerea, în ansamblul fenomenelor ei, nu poate avea loc în afara interacţiunii adecvate gonadotropină corionică - receptor, fapt ce condiţione...
Sarcină ectopică în corn rudimentar: diagnostic precoce şi management
Sarcina în corn rudimentar este o entitate clinică rară, cu o incidenţă ce variază între 1:76.000 şi 1:140.000 de sarcini. Simptomatologia care îns...
Relaţia dintre cicatricea uterină determinată de intervenţii histeroscopice şi abdomenul acut chirurgical în sarcină - prezentare de cazuri -
Abdomenul acut chirurgical în cursul sarcinii reprezintă o entitate patologică, plurietiologică, cu evoluţie rapidă şi risc vital atât pentru partu...
Impactul psihoemoţional al sarcinii ectopice – experienţa clinicii noastre
Introducere. Studiul de faţă a avut drept scop identificarea şi evaluarea impactului psihoemoţional al femeilor care au fost diagnosticate cu sarci...