HIV diagnoses
In 2016, a total of 29444 new HIV diagnoses were reported by the 31 countries of the EU/EEA, with a rate of 5.9 per 100 000 when adjusted for reporting delay. The highest rates were reported by Latvia (18.5; 365 cases), Estonia (17.4; 229 cases), and Malta (14.5; 63 cases). The lowest rates were reported by Slovakia (1.6; 87 cases) and Hungary (2.3; 228 cases).
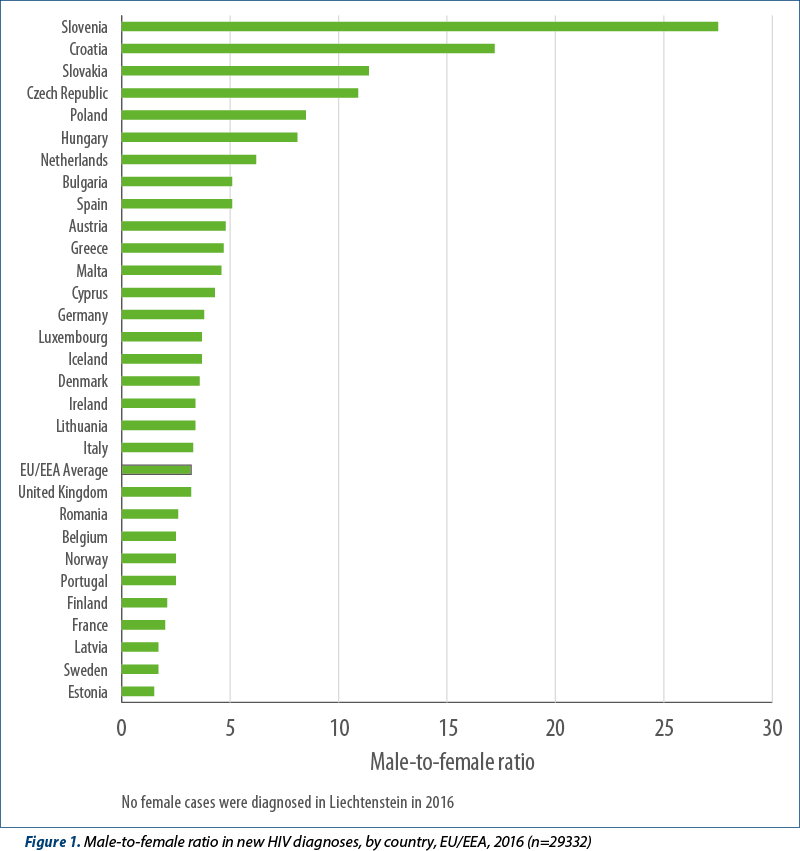
The overall rate for men diagnosed with HIV in the EU/EEA was 8.9 per 100 000 population, and for women it was 2.6 per 100 000 population, resulting in a male-female ratio in 2016 of 3.2. This ratio was highest in Slovenia (27.5), Croatia (17.2), Slovakia (11.4), and the Czech Republic (10.9) (Figure 1). The predominant mode of transmission in these countries was sex between men (Figure 5).
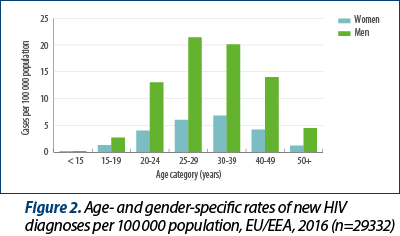
Men had higher age-specific rates than women in all age groups except among persons under 15 years old, where age-specific rates were similar (Figure 2). The highest overall age-specific rate of HIV diagnoses was observed among 25-to-29-year-olds (13.9 per 100 000 population) with the rates for men also peaking in this age group at 21.4 per 100 000 population, while rates for women were highest in the 30-39-year age group (6.8 per 100 000 population) - Figure 2.
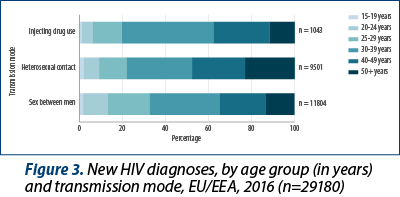
The median age at diagnosis was lower for MSM (34 years old) than for cases attributed to injecting drug use (36 years old) or heterosexual transmission (39 years old). The 30-39-year-age group accounted for most HIV diagnoses overall (32%) and in all transmission groups (43% among cases attributed to injecting drug use; 33% among cases attributed to sex between men; 30% among cases attributed to heterosexual transmission) (Figure 3). Thirty-four percent of cases attributed to sex between men (MSM) are diagnosed before the age of 30, while half (48%) of HIV infections due to sex between men and women are diagnosed at 40 years or above, and nearly one-quarter (23%) at 50 years or above.
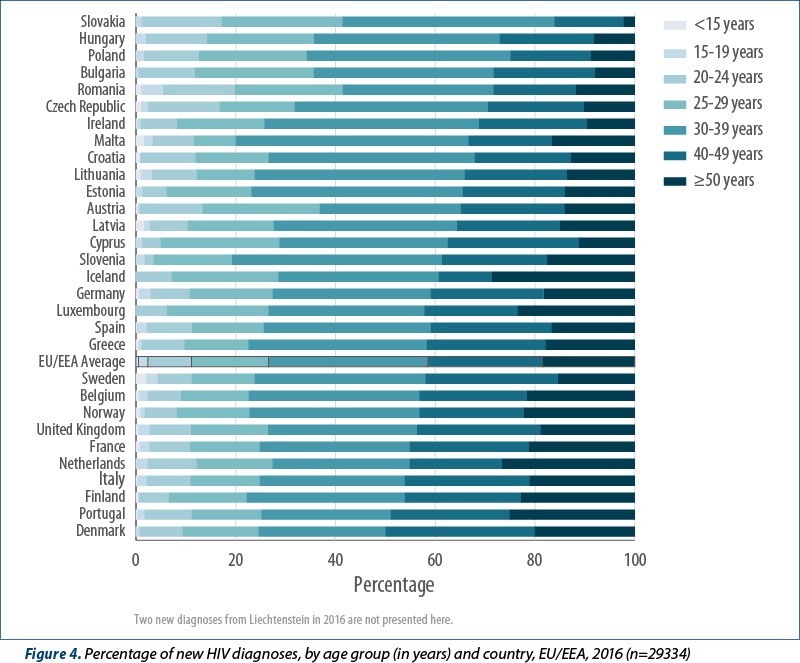
Young people aged 15 to 24 years comprised 12% of the EU/EEA population and 11.1% of HIV diagnoses in 2016. The Czech Republic and Slovakia reported more than15% of their HIV diagnoses in this age group (Figure 4). In total, 39% of the EU/EEA population are considered to be older adults (50 years and above) and they contributed 18.5% of new HIV diagnoses reported in 2016. In nine countries (Belgium, Finland, France, Iceland, Italy, Luxembourg, Netherlands, Norway, Portugal) older adults comprised more than 20% of those newly diagnosed with HIV.
Data on transmission mode provide information on the groups that are most affected by HIV in the EU/EEA:
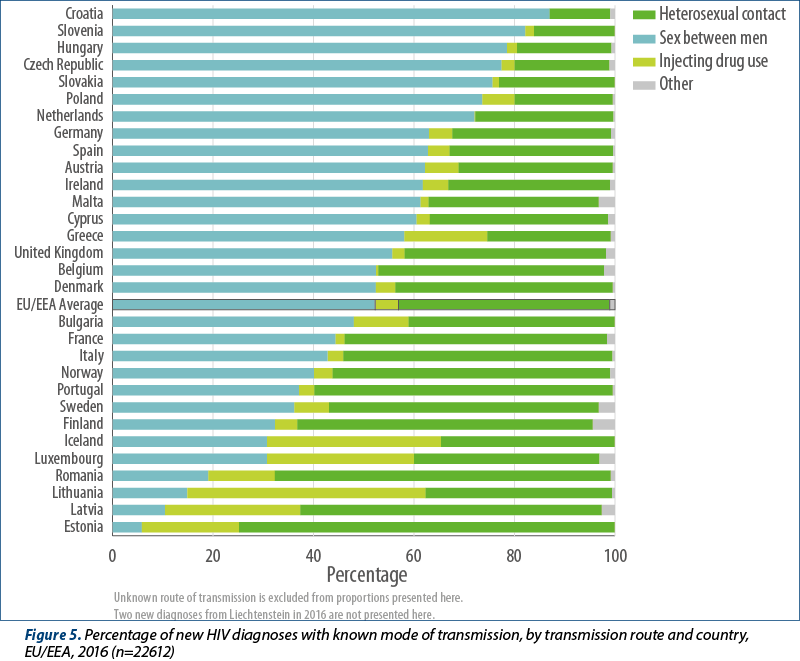
As in recent years, sex between men remains the predominant mode of HIV transmission reported in the EU/EEA, accounting for 40% (11819) of all new HIV diagnoses in 2016, and in more than half (53%) of diagnoses the route of transmission was known (Figure 5). Among those with known route of HIV transmission, sex between men was the most commonly reported route of transmission, and accounted for more than 60% of new HIV diagnoses in 13 countries (Austria, Croatia, Cyprus, the Czech Republic, Germany, Hungary, Ireland, Malta, the Netherlands, Poland, Slovakia, Slovenia, and Spain) (Figure 5).
Sex between men and women is the second most commonly reported mode of transmission in the EU/EEA, accounting for 32% (9510) of HIV diagnoses and 42% of diagnoses where the route of transmission was known (Figure 5). Heterosexual transmission is the most commonly reported known mode of transmission in nine EU/EEA countries (Estonia, Finland, France, Italy, Latvia, Norway, Portugal, Romania and Sweden). More than one-third (39%; 2595) of newly diagnosed cases are among heterosexual migrants originating from countries with generalised HIV epidemics. The highest proportions of these were observed in Ireland (65%), Germany (58%), Luxembourg (54%) and France (50%).
Four per cent overall and five per cent (1044 cases) of HIV diagnoses with known route of HIV transmission reported were attributed to injecting drug use (Figure 5). Injecting drug use was the probable route of transmission for one quarter or more of the cases reported in Lithuania (47%), Iceland (35%), Latvia (27%) and Luxembourg (29%) (Figure 5).
Of the remainder, 150 diagnoses (less than 1%) were reported as due to mother-to-child transmission; however, 113 of these cases (75%) were born outside the country in which the case was later reported. In addition, seventy-six diagnoses were reported to be due to contaminated transfusion of blood and its products, and 13 cases were reported to be hospital-acquired infections. Nearly all of these nosocomial cases were reported to have been acquired outside the country where the case was reported.
Transmission mode was reported as „unknown“ for 6832 diagnoses (23%) with wide variation among countries: less than 5% of diagnoses were reported as „unknown“ in Bulgaria, Croatia, the Czech Republic, Luxembourg, Malta, Norway, Portugal, Romania and Slovenia, and over 60% were reported as unknown in Poland.
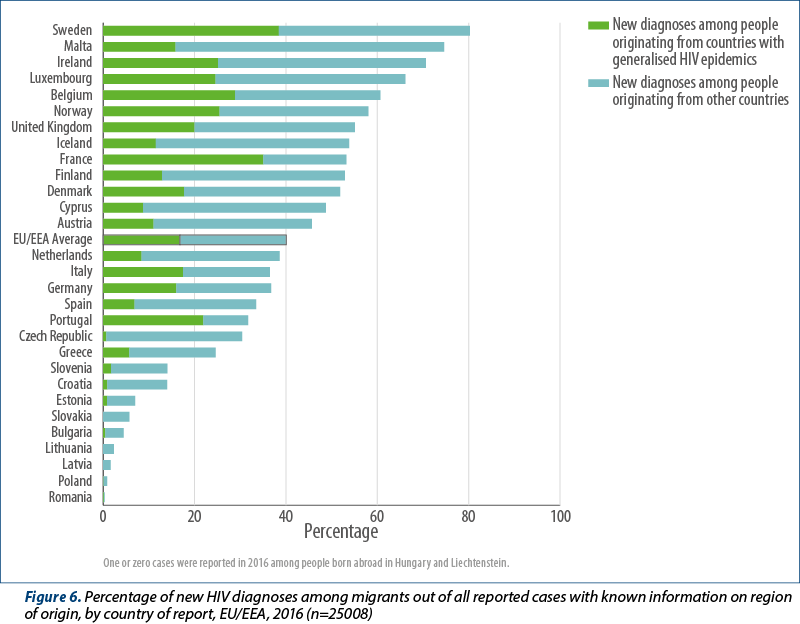
In 2016, 30 EU/EEA countries provided information on the country of birth, country of nationality, or region of origin for 25 008 (87%) HIV diagnoses (Figure 6). In the EU/EEA, 10021 diagnoses (40% of those with known information on region of origin) were made among people originating from outside of the reporting country. Of these, 4206 diagnoses (17% of those with known information on region of origin), irrespective of transmission mode, were among people originating from countries with generalised HIV epidemics (Figure 6). An additional 23% of new diagnoses with known region of origin (5815 cases) were among people born outside of the reporting country, but did not originate from a country experiencing a generalised epidemic. Countries with at least half of their new HIV diagnoses among people originating from outside of the reporting country were Sweden (80%), Malta (75%), Ireland (71%), Luxembourg (66%), Belgium (61%), Norway (58%), the United Kingdom (55%), Iceland (54%), Finland (53%), France (53%), and Denmark (52%).
Thirteen EU/EEA countries (Bulgaria, Croatia, Cyprus, Czech Republic, Denmark, France, Ireland, Iceland, Malta, Norway, Slovenia, Slovakia and Sweden) reported data on whether the case diagnosed in 2016 was diagnosed in another country or setting previously. About 11% of new diagnoses in 2016 in those countries (3% of the EU/EEA total) were reported to have been previously diagnosed. The proportion of previous positives among 2016 diagnoses varied between countries: Croatia (5%), Cyprus (16%), Czech Republic (12%), Denmark (30%), France (7%), Ireland (34%), Malta (22%), Norway (17%), Slovakia (2%), Slovenia (3%), and Sweden (27%).
Information on CD4 cell count at the time of HIV diagnosis was provided by 26 countries, for 18282 (67%) adults and adolescents diagnosed in those countries. All countries reporting such data were able to provide CD4 cell counts for over 50% of their reported cases, apart from Lithuania and Germany, which provided data for 39% and 23% of cases, respectively. Nearly half (48%) of all cases with a CD4 cell count available were considered to have been diagnosed several years after being infected, with a count of less than 350 cells per mm3, including 28% of cases considered to have advanced HIV infection (CD4<200 cells/mm3). The proportion of those diagnosed late, with a CD4 count lower than 350 cells per mm3, was above 50% in eight countries: Lithuania (66%), Romania (64%), Greece (58%), Croatia (56%), Italy (56%), Estonia (54%), Finland (52%) and Germany (51%).
Among all cases diagnosed where a CD4 cell count was available, 20% (3537) had a CD4 cell count between 350 and 500 cells per mm3 and 32% (5880) had a CD4 cell count above 500 cells per mm3 (data not shown), indicating more recent infection. When analysing CD4 cell count by transmission mode, higher proportions of people presenting at a later stage of HIV infection (CD4<350 cells/mm3) were observed among women (53%); older adults (54% in 40‑49 year-olds and 63% in persons over 50 years); men and women infected by heterosexual sex (63% and 54%, respectively); people who acquired HIV through injecting drug use (50%) and migrants from south and south-east Asia (53%) and sub-Saharan Africa (57%) (Figure 7).
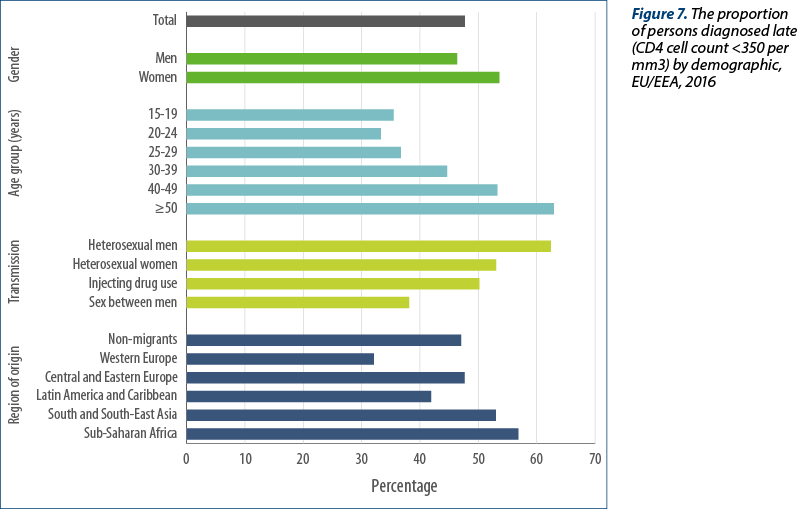
The lowest proportions of late diagnosis, indicated by CD4 counts below 350 cells per mm3 at diagnosis, were observed among younger age groups (36% of 15-19 year olds, 33% of 20-24 year olds), men who acquired HIV through sex with another man (38%), and migrants from other western European countries (32%).
Trends in HIV diagnoses
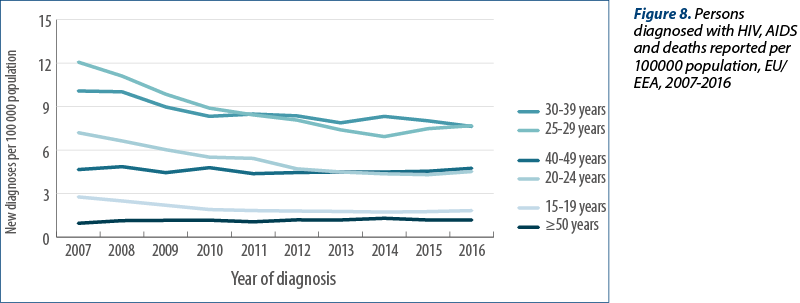
The trend in reported HIV diagnoses for the period 2007-2016 has remained relatively stable, with a slight decline observed during recent years. In the earlier part of this period, rates were 6.8 and 6.9 per 100 000, decreasing slightly to 6.5 in more recent years, and 5.9 in 2016 (30523 cases when adjusted for reporting delay; see Figure 8). In the HIV/AIDS surveillance report on 2015 data(1), 29747 HIV diagnoses were reported for 2015, but after Member States updated their historical data, this number increased by over 3 000 cases and may still increase further in similar updates over the next one to two years.
While the overall EU/EEA trend has remained somewhat stable over the last decade, trends at national level are contrasting. For the first time in recent years, several countries have reported a decline in new HIV diagnoses, even after adjusting for reporting delay. These include: Austria, Belgium, Denmark, Estonia, France, Italy, the Netherlands, Norway, Spain and the United Kingdom. On the other hand, since 2006, and taking reporting delay into account, rates of HIV diagnoses have more than doubled in Croatia, the Czech Republic, Hungary, Lithuania, Malta and Slovakia, and have increased by over 50% in Bulgaria, Cyprus, Poland, Romania and Slovenia. Reporting delay affects some countries more than others, and therefore the decreases in the rates of new HIV diagnoses may be overestimated and the increases in rates may be underestimated.
Trends differ by gender and age group. Age-specific rates in women under 40 years old have steadily declined since 2007, while rates among women over 40 years have been stagnant and those above 50 have increased. Among men, rates in all age groups increased overall during the period, in most cases peaking in 2015 (Figures 9a and 9b). Rates in men aged 20-39 years old declined between 2015 and 2016, while rates among men aged 15-19 years old remained stable and rates among men aged 50 and above increased.
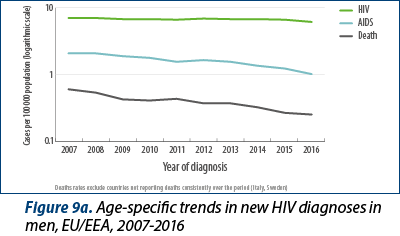
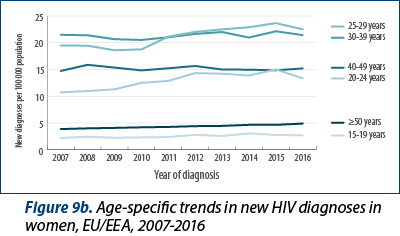
Over the last decade, the median age at HIV diagnosis increased from 35 years old in 2007 to 37 years old in 2016 overall, from 32 to 37 years old among women and from 36 to 37 years old among men. A larger proportion of diagnoses are being reported in the older age groups; 13% of persons diagnosed in 2007 were over 50 years at HIV diagnosis and this rose to 19% of those diagnosed in 2016. In women, 9% of diagnoses in 2007 and 18% in 2016 were made in persons aged 50 years old or above, while in men 15% of diagnoses in 2007 and 19% in 2016 were made in persons aged 50 years or above (data not shown).
Since 2007, 29 EU/EEA countries have consistently reported data on the transmission mode. Data from Estonia and Poland were excluded in the analysis below as more than 50% of their data on transmission mode were missing. Data from Spain and Italy were also excluded because coverage by the surveillance system has been gradually expanding on a national basis over the last decade. Data on the transmission mode from those countries consistently reporting (Figures 10a, 10b and 11) indicate the following:
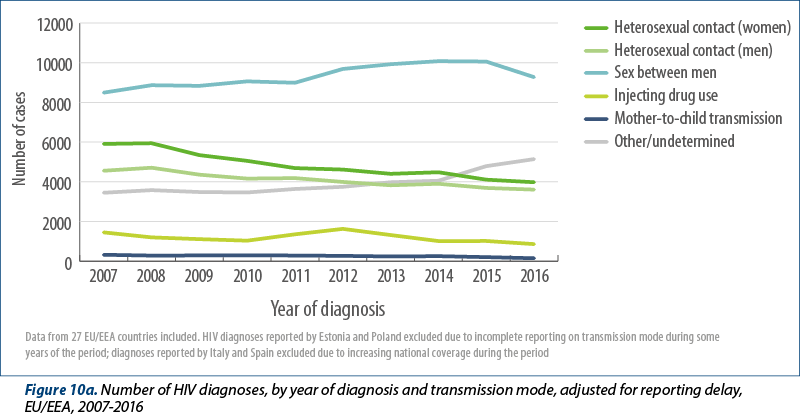
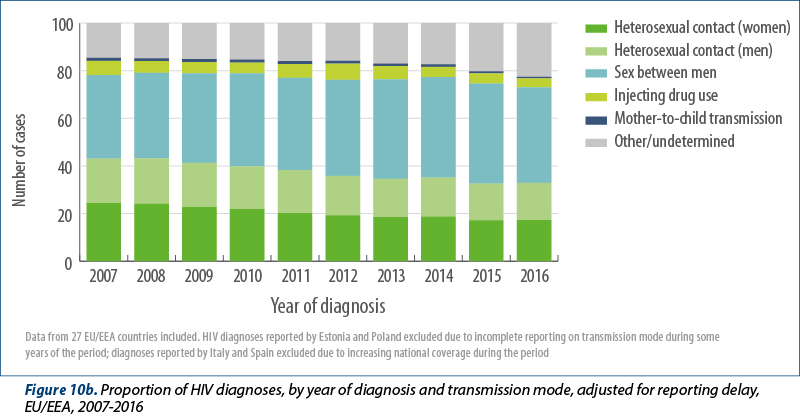
The proportion of all HIV diagnoses attributed to sex between men increased over the period from 35% of cases in 2007 decreasing to 40% in 2016. The number of HIV diagnoses reported among MSM in these countries, adjusted for reporting delay, increased from 8493 cases in 2007 and peaked at 10079 cases in 2014. Although fewer cases were reported in 2016 (9274), additional reporting delay which could not be accounted for probably plays a partial role in this decline. Most of the decline appears to be due to fewer diagnoses among MSM in the following countries: Austria, Belgium, Italy, the Netherlands and the United Kingdom. During years where the surveillance system coverage was comparable, this decline was also noted for Spain. Between 2007 and 2016, increases were observed in the majority of EU/EEA countries, with substantial increases noted in Bulgaria, Croatia, Cyprus, Czech Republic, Hungary, Ireland, Lithuania, and Malta in recent years. Cases attributed to MSM born outside of the reporting country did not appear to decline during 2015-2016 in the same way as observed in EU/EEA-native MSM (Figure 11).
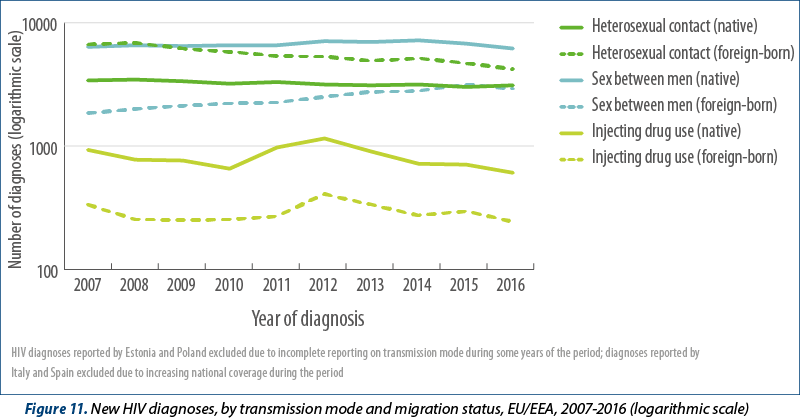
The adjusted number of heterosexually acquired cases decreased steadily from 10465 in 2007 to 7585 in 2016 (Figure 9a). The proportion of all HIV diagnoses attributed to sex between men and women decreased from 43% of cases in 2007 to 33% in 2016 (Figure 10b). Between 2007 and 2016, the number of cases among women and foreign-born heterosexuals decreased at a greater rate than cases among men and non-foreign-born people (Figures 10a and 11). The decline in foreign-born cases is mainly due to sharp decreases among migrants originating from countries with generalised HIV epidemics (5873 in 2007; 3388 in 2016).
The number of HIV diagnoses reported among people who inject drugs has also declined since 2007 (from 1450 cases to 860 cases) in both foreign-born and non-foreign-born people who inject drugs (Figure 10a; Figure 11).
A temporary increase in overall numbers for the EU/EEA was observed in 2011 and 2012 due to localised outbreaks reported in Greece and Romania, but in 2016 the overall downward trend in the number of reported cases continued for the EU/EEA. Although diagnoses due to injecting drug use nearly doubled between 2015 and 2016 in Lithuania, Estonia, Italy, Latvia, and Portugal in particular, we have seen a sharp decrease in the number of HIV diagnoses due to injecting drug use over the last decade.
The number of diagnoses reported to be due to HIV transmitted from mother to child decreased from 322 in 2007 to 147 in 2016 (Figure 10a). A large and growing proportion of these cases originated in migrants (69% in 2007 and 75% in 2016).
The number of HIV diagnoses reported to be due to nosocomial infection has remained stable over this period, with 18 cases in 2007 and 12 in 2016. The number of cases reported to be due to contaminated transfusion of blood and its products has decreased from 77 in 2007 to 66 cases in 2016. A large and growing proportion of these cases were among people who had migrated to the EU/EEA and were later diagnosed in the reporting country (61% in 2007 and 83% in 2016).
The number of cases with an unknown mode of transmission has increased from 3448 in 2007 to 5142 cases in 2016 (14% of cases in 2007 and 23% in 2016). This increase is affected by reporting delay and will probably decrease slightly in future reporting.
Reporting delays differ significantly among transmission categories for some countries. When standardised adjustments for reporting delay are introduced, these increase the number of reported HIV cases in all transmission categories by between 8% and 19%, depending on the category. Figures 10a and 10b show these adjusted trends.
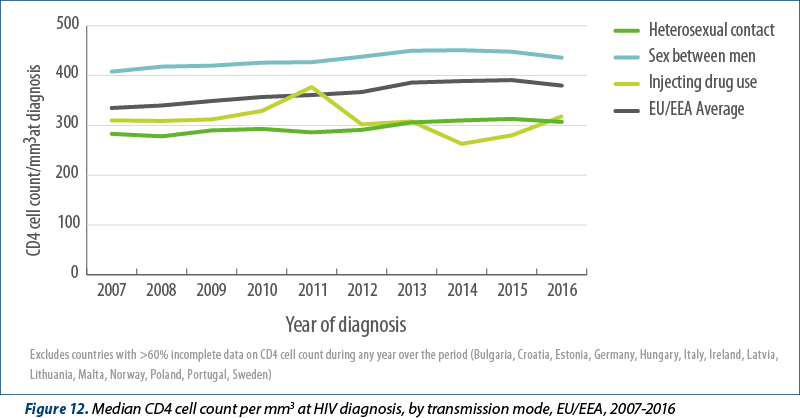
While many people are still diagnosed late, several years after being infected with HIV, the median CD4 cell count at HIV diagnosis has increased significantly over the past decade, from 335 (95% CI 330-340) cells/mm3 in 2007 to 380 (95% CI 375–385) cells/mm3 in 2016, indicating improvements in case ascertainment due to more effective testing policies. The group with the highest median CD4 cell count at diagnosis is MSM, with 440 cells/mm3 in 2016. However, this has also improved over the last decade, indicating earlier diagnosis (Figure 12). Median CD4 count at diagnosis was lower in cases attributed to heterosexual transmission, but similarly increased over the period (from 283 cells/mm3 in 2007 to 307 cells/mm3 in 2016).
AIDS cases, morbidity and mortality
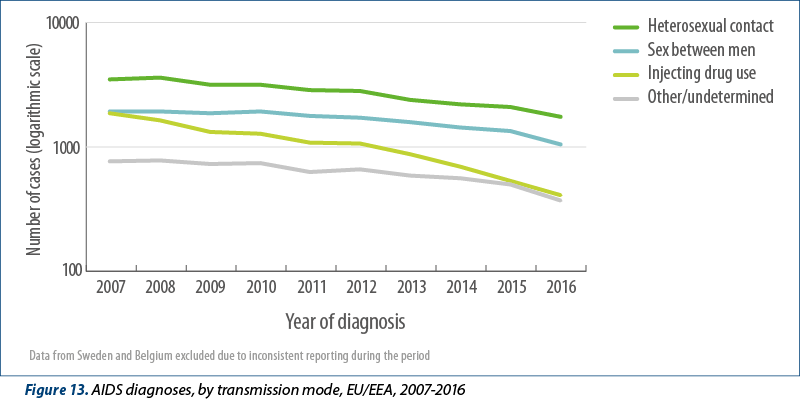
Despite improvements in early diagnosis of HIV, 3628 diagnoses of AIDS were reported by 29 EU/EEA countries in 2016, giving a rate of 0.8 cases per 100 000 population. The highest rates were reported by Latvia (5.8; 114 cases), Estonia (3.1; 41 cases), and Portugal (2.5, 261 cases) and overall, 68% of these AIDS diagnoses were made within 90 days of the HIV diagnosis, indicating that the majority of AIDS cases in the EU/EEA are due to late diagnosis of HIV infection. The rate of reported AIDS cases has halved in the last decade, from 1.6 per 100 000 (7 938 cases) reported in 2007. This decline is noted in all transmission groups but appears greatest among cases attributed to heterosexual transmission and injecting drug use (Figure 13). Despite the general EU/EEA-wide decline, since 2007 an increase has been reported in the rate of AIDS diagnoses in Bulgaria, Hungary, Latvia and Lithuania.
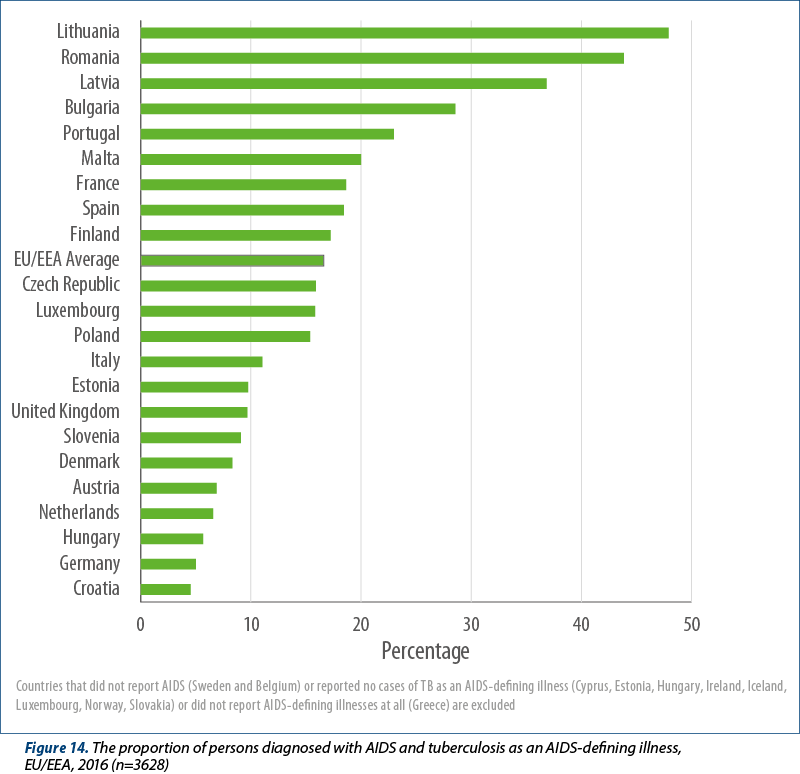
In the EU/EEA, the most common AIDS-indicative diseases diagnosed in 2016 were Pneumocystis pneumonia (20%), pulmonary and/or extra-pulmonary tuberculosis (15%), oesophageal candidiasis (11%), and wasting syndrome due to HIV (10%). Twenty-two countries reported tuberculosis (TB) (pulmonary and/or extra-pulmonary) as an AIDS-defining illness in persons newly diagnosed with AIDS in 2016. In these countries, 16% of people diagnosed with AIDS presented with TB as an AIDS-defining illness, ranging from 5% or less (Croatia and Germany) to more than 40% of cases (Lithuania and Romania) (Figure 14).
Twenty-nine EU/EEA countries (all but Italy and Sweden) reported data on deaths of individuals diagnosed with AIDS. Overall, 849 individuals were reported to have died due to AIDS-related causes during 2016, although this data is impacted by under-reporting due to the challenges in many countries in linking to death registries. Nevertheless, AIDS-related deaths reports have been consistently decreasing since 2007, when 2172 deaths were reported, suggesting improvements in linkage to care and treatment, although delays in reporting and underreporting may affect the latest figures (Figure 8). From the beginning of the HIV epidemic to the end of 2016, a cumulative total of 354133 individuals have been diagnosed with AIDS in the EU/EEA. The cumulative total of cases reported as known to have died due to AIDS-related causes by the end of 2016 was 170015, while an additional 19418 persons who were living with HIV are known to have died of non-AIDS related causes.
Conclusions
HIV surveillance data for 2016 contribute to demonstrating important changes in the epidemiology of HIV in EU/EEA countries over the past decade. In the EU/EEA as a whole, the rates of AIDS and AIDS-related deaths have decreased significantly over the past decade, reflecting greater access to treatment and better case management. For the first time in a decade, there appears to be a slight decline in the rate of new HIV diagnoses per 100 000 population in recent years, with an adjusted rate of 5.9 per 100 000 population reported in 2016. While the notification rate is lower than in previous years, it is expected to be revised upwards in future reporting cycles due to reporting delay, which is common for HIV generally and for certain countries in the EU/EEA in particular. Despite the evidence of some progress in reducing the number of new HIV diagnoses in the EU/EEA overall, the rates continue to increase markedly in one-third of EU/EEA countries.
For the first time in 2016, there appears to be evidence of a true decrease in HIV diagnoses among men who have sex with men in select EU/EEA countries and this appears to be driving the overall decline observed in the EU/EEA. This is significant because MSM account for the largest number of new HIV diagnoses in the EU/EEA and this has been the only population in the EU/EEA in which HIV cases have increased steadily during most of the last decade. Decline at EU/EEA level is driven by substantial decline in specific EU/EEA countries, namely Austria, Belgium, Italy, the Netherlands, Spain and the United Kingdom. Reasons for the decrease may include successful programmes to offer more frequent and targeted HIV testing to promote earlier diagnosis, rapid linkage to care and immediate initiation of antiretroviral treatment for those found to be positive(1,2). While still not implemented widely in Europe, the use of formal and informal pre-exposure prophylaxis may also have played a role in the decline of HIV diagnoses observed in at least some of these settings(2,3).
However, the positive trend described above is countered by the prevailing situation in other EU/EEA countries where HIV continues to increase among MSM, with substantial increases reported in Bulgaria, Croatia, Cyprus, Czech Republic, Hungary, Ireland, Lithuania, and Malta in recent years. Similarly, in these countries and more widely in the EU/EEA, new HIV diagnoses in migrant MSM continue to increase. There is an urgent need to significantly scale up more effective combination prevention programmes for this at-risk population. This includes promoting the uptake of regular, easy-to-access HIV testing, accompanied by immediate linkage to care and treatment for those found positive; condoms, peer support and possible pre-exposure prophylaxis for some populations of high-risk HIV-negative men(4).
An important epidemiological trend observed over the past decade has been the substantial decrease in the number of HIV infections transmitted through heterosexual contact, particularly among women. However, heterosexual transmission still remains the second most common mode of HIV transmission reported in the EU/EEA and is the most common transmission mode in some countries. Part of this declining trend in heterosexual cases is probably influenced by the decline (since 2007) in the number of heterosexually-acquired cases in migrants originating from countries with generalised HIV epidemics(5). Nonetheless, in 2016, migrants (or persons originating from outside of the reporting country) again constituted a considerable proportion (40%) of new HIV diagnoses in the EU/EEA. It is important to recognise the emerging evidence that a significant proportion of migrants, even those originating from high HIV-endemic areas, acquire HIV after the arrival in the EU/EEA(6-8). This indicates the need for targeted prevention directed at this vulnerable population group from the moment of their arrival.
Transmission among people who inject drugs continues to decline and remains at a low level in most EU/EEA countries, thanks to well-established harm reduction programmes throughout most of the region. However, sudden increases have been observed in recent years in Romania and Greece – countries with previously very low levels of HIV among people who inject drugs(9,10) – and more recently localised outbreaks have been reported in Ireland and Scotland(11,12). This reinforces the importance of maintaining adequate scale and coverage of harm reduction services and recognising that trends can change quickly in this at-risk group, in the absence of effective prevention delivered at scale(13).
Despite clear evidence of the benefits of introducing antiretroviral treatment early for the health of the HIV-positive individual(14,15) and the fact that this should serve as an incentive to know one’s HIV status, many people continue to be diagnosed with HIV years after becoming infected and are only diagnosed when they reach an advanced stage of illness. It is estimated that there were 120 000 people living with undiagnosed HIV in the EU/EEA in 2015, implying that about 15% of those living with HIV are not aware of their status(16). In addition to the clinical and personal benefits for the individual diagnosed, early diagnosis and treatment can also benefit sexual and injecting partners by inhibiting onward HIV transmission. Nearly half of those diagnosed (48%) have a CD4 cell count of less than 350 cells per mm3 at diagnosis, including 28% of cases with advanced HIV infection (CD4 <200 cells/mm3), indicating the need to diversify and improve testing programmes to diagnose people living with HIV (PLHIV) at an earlier stage. Furthermore, while AIDS cases continue to decline in the EU/EEA, 68% of the AIDS cases reported in 2016 were diagnosed at the same time or shortly after being diagnosed with HIV. This is a clear indication that these individuals were infected many years previously and suggests problems with access to, and uptake of HIV testing for those most at risk.
One of the sub-groups that have emerged with the highest rate of late diagnosis are older adults (persons aged over 50 years), in particular older men reported as having acquired HIV heterosexually. During the last decade, there has been a trend towards increasing median age at HIV diagnosis, particularly among women. In 2016, nearly one in five new HIV diagnoses was among a person over 50 years of age. This may be the result of stigma, or low or inaccurate risk perception among older adults themselves or the healthcare providers who serve them. Increased HIV testing targeting this group, particularly risk-based screening and indicator-condition testing, may reduce late diagnosis in this population(17).
In recent years, there has been a worrying trend of reduced data completeness on the HIV transmission route, with nearly one-quarter of cases reported in 2016 lacking information on probable route of HIV transmission. While this proportion may have been affected by the introduction of an earlier 2016 reporting deadline, the trend had been evident in recent years. Information on probable route of transmission is crucial to better inform HIV prevention interventions and programme planning. Greater efforts to improve collaboration with clinicians and follow up with other data providers may improve the transmission data. Meanwhile, statistical adjustments for missing data will be explored(18).
The changing epidemiology of HIV infections observed in the EU/EEA over the last decade suggests that some progress has been achieved, particularly with regard to reducing infections attributed to heterosexual transmission and injecting drug use and more recently the decline of HIV resulting from sex between men in a few EU/EEA countries. However, these epidemiological trends also indicate that it is crucial to sustain, and in some places strengthen evidence-based HIV prevention interventions tailored to the local epidemiological context and targeting those most at risk. Programmes on the prevention and control of HIV infection adapted to key populations and maintained to scale remain important in EU/EEA countries. For most EU/EEA countries, this means a strong focus on MSM, including intra-European and other migrant men who have sex with men. Other migrants, both those from countries with generalised HIV epidemics and others, are also a key vulnerable population that needs specific prevention and control efforts in the majority of EU/EEA countries. Given the increasing evidence of post-migration HIV acquisition, it is important that migrant-sensitive services for prevention and HIV testing, combined with policies which promote and ensure linkage and access to care, are delivered in all EU/EEA countries. Finally, harm reduction programmes among people who inject drugs and their sexual partners are crucial and should be maintained and scaled up where service coverage is low, particularly when pat- terns of drug use change.
Acknowledgement: We would like to acknowledge ECDC for the very good document published, with high quality data and a permissive policy of reproduction.
ECDC Copyright and Limited Reproduction Notices