Objective. Oocyte cryopreservation is being offered to women who wish to defer childbearing. Elective oocyte cryopreservation provides women the possibility to prevent involuntary childlessness due to age-related infertility. The purpose of this review is to summarize recent data regarding the outcomes and economic implications of elective oocyte cryopreservation. Recent findings. Oocyte vitrification has comparable in vitro fertilization (IVF) outcomes as fresh oocytes. Although evidence about the outcomes of IVF cycles in the population who undergoes elective oocyte vitrification is limited, new studies are starting to emerge. The age at retrieval and the number of available oocytes are the most important factors that improve a woman’s chance of having a baby. Biologically, the ideal age of cryopreserving is <35 years old. However, the majority of studies show that elective fertility preservation is more cost-effective at 37-38 years old. When counseling women who take into consideration postponing motherhood, they should be informed of the complications associated with pregnancy at an advanced maternal age. Conclusions. Elective oocyte cryopreservation is a strategy that helps women gain the reproductive autonomy they need for deferring childbearing. Given the increasing interest toward elective oocyte cryopreservation, clinicians need to properly counsel and inform women about the limitations of this procedure. Oocyte vitrification does not guarantee success, but increases the likelihood of having a child later in life.
Crioprezervarea electivă de ovocite: putem prelungi perioada de viaţă fertilă a femeilor?
Elective oocyte cryopreservation: can we expand the women’s reproductive lifespan?
First published: 23 decembrie 2020
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/ObsGin.68.4.2020.4022
Abstract
Rezumat
Obiectiv. Femeile care doresc să amâne concepţia au posibilitatea de a crioprezerva ovocite. Acestea pot fi utilizate la o vârstă mai înaintată, atunci când femeile decid să obţină o sarcină. Crioprezervarea electivă de ovocite le oferă femeilor şansa de a preîntâmpina infertilitatea cauzată de vârsta maternă avansată. Această recenzie a literaturii are ca scop sintetizarea celor mai recente studii privind ratele de succes ale crioprezervării elective de ovocite, respectiv implicaţiile financiare inerente. Constatări recente. Procedurile de fertilizare in vitro (FIV) cu ovocite vitrificate au rezultate similare cu ale procedurilor efectuate cu ovocite proaspete. Informaţiile privind succesul şedinţelor de FIV la pacientele care au crioprezervat ovocite electiv sunt limitate, însă noi studii despre acest subiect încep să apară. Cei mai importanţi factori care influenţează şansele unei femei de a avea un copil sunt vârsta la momentul prelevării de ovocite şi numărul de ovocite vitrificate. Din punct de vedere biologic, vârsta ideală pentru crioprezervare este sub 35 de ani. Cu toate acestea, din punctul de vedere al cost-eficienţei, majoritatea studiilor arată că vârsta indicată pentru prezervarea electivă de ovocite este de 37-38 de ani. Atunci când clinicienii consiliază o femeie privind amânarea concepţiei primului copil, este necesar ca aceasta să fie informată despre complicaţiile asociate unei sarcini la o vârstă înaintată. Concluzii. Crioprezervarea electivă de ovocite este o procedură strategică prin care femeile îşi pot exercita autonomia reproductivă, oferindu-le posibilitatea de a-şi extinde fertilitatea. Având în vedere tendinţa tot mai mare a femeilor de a-şi dori copii la o vârstă mai târzie, cât şi interesul crescut pentru crioprezervarea de ovocite, clinicienii au datoria să consilieze şi să informeze femeile privind limitările acestei proceduri. Deşi vitrificarea de ovocite nu garantează succesul concepţiei, aceasta creşte şansele unei femei de a avea un copil la o vârstă mai înaintată.
Introduction
Elective oocyte cryopreservation (EOC), also known as social egg-freezing, was defined by the ANZSREI consensus as a “a strategy to improve a woman’s longitudinal fertility potential with her own oocytes in the absence of a medical diagnosis of infertility or contraindication to pregnancy”(1).
Originally, cryopreserved oocytes were used for women with a medical need for these procedures, such as patients diagnosed with premature ovarian insufficiency, endometriosis, or those who underwent oophorotoxic cancer treatment. Subsequently, the opportunity rose to cryopreserve oocytes solely for elective fertility preservation (EFP) purposes. This seems to overcome the age-related infertility issue, a growing problem in our current society.
Elective oocyte cryopreservation offers women the possibility to prevent involuntary childlessness due to age-related infertility. Furthermore, women can have children who are biologically related to them, in contrast to the other options that are available such as in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI) with donor oocytes.
In the past years, there has been an increasing number of women who wished to delay childbearing because of different personal reasons. The main problem which occurs for these women is the decreasing fertility that comes with aging. EOC is a strategy that helps women gain the reproductive autonomy they need for deferring childbearing. This is both an opportunity and a challenge for the healthcare provider because these women need proper counseling. This strategy is costly and can raise false hopes. For this reason, women should be accurately informed and have realistic expectations before taking a decision.
The average age of women who have their first child is increasing. Women choose to defer childbearing because of the following reasons: the absence of a partner (this being the main reason), seeking higher education, career prioritization, financial reasons, or psychological reasons such as not being prepared for parenthood(2).
It is known that both ovarian reserve and oocyte quality decrease with age. Fertility in women starts to decrease gradually beginning with the age of 32 years old and declines steeply after the age of 37(3). Simultaneously, the risk of miscarriage increases abruptly, from approximately 11% in the third decade of life to 93% over the age of 45 years old(4). This results in a rise of involuntary childlessness. The risk of involuntary childlessness increases from 2% to 3% for women younger than 30 years old, to 36% for women of 40 years or older(5).
Habbema et al. created a simulation that took into account the age-related fertility decline and the IVF success rates as a means to determine the ideal age of starting a family for a couple to achieve their desired family size. The simulation proposed that, in order to have a chance of at least 90% to conceive, couples should start trying to conceive when the female partner is 35 years old or younger, in case IVF is an acceptable option. To conceive two or three children, the conception should begin when the female partner is 31 or 28 years of age, respectively. If the couple does not accept IVF, they should start no later than the age of 32 years old for a one-child family, at 27 years old for a two-child family, and at 23 years old for having three children(6).
After slow freeze protocols of oocytes have been replaced with vitrification, emerging evidence has shown that IVF with cryopreserved oocytes is both safe and has comparable pregnancy rates as IVF/ICSI with fresh oocytes(7-9). In 2013, this led the American Society for Reproductive Medicine to remove the experimental status of oocyte cryopreservation when this procedure is medically indicated for fertility preservation. However, they report a lack of data supporting the “safety, efficacy, ethics, emotional risks, and cost-effectiveness of oocyte cryopreservation” when it is used for the sole purpose of deferring childbearing(10). On the other hand, the European Society of Human Reproduction and Embryology stated that “oocyte cryopreservation should not just be available for women at risk of premature pathogenic or iatrogenic fertility loss, but also for those who want to protect their reproductive potential against the threat of time”(11).
Currently, oocyte cryopreservation is receiving increasing promotion and public acceptance. Therefore, this review has the purpose to evaluate the existing data regarding the birth outcomes, efficiency and the costs of elective oocyte cryopreservation, and aims to guide clinicians working with women considering elective oocyte cryopreservation.
Outcomes of elective oocyte cryopreservation
Most data available today regarding the outcomes of IVF derive from IVF using donor oocytes, which come from young women and have a survival rate of over 95%(9). This is not the case for EOC, because women choosing EOC are usually over 35 years old at the time of oocyte retrieval. The oocytes have a poorer quality and are less resistant to the freeze-warming process than oocytes from the younger oocyte donor population. Therefore, women choosing to cryopreserve oocytes electively need a higher number of oocytes per pregnancy achieved than donor oocytes(12).
The evidence is scarce in literature about the outcomes of IVF cycles in the population who undergoes elective oocyte vitrification. On one hand, this is a relatively new concept and, on the other hand, women who cryopreserved their oocytes haven’t yet decided to return and use them.
Table 1 and Table 2 present the success rates of IVF conducted with cryopreserved oocytes for elective nonmedically-indicated fertility preservation in three studies(12-14). They all concluded that the age at retrieval and the number of available oocytes are the most important factors that increase a woman’s chance of having a baby.
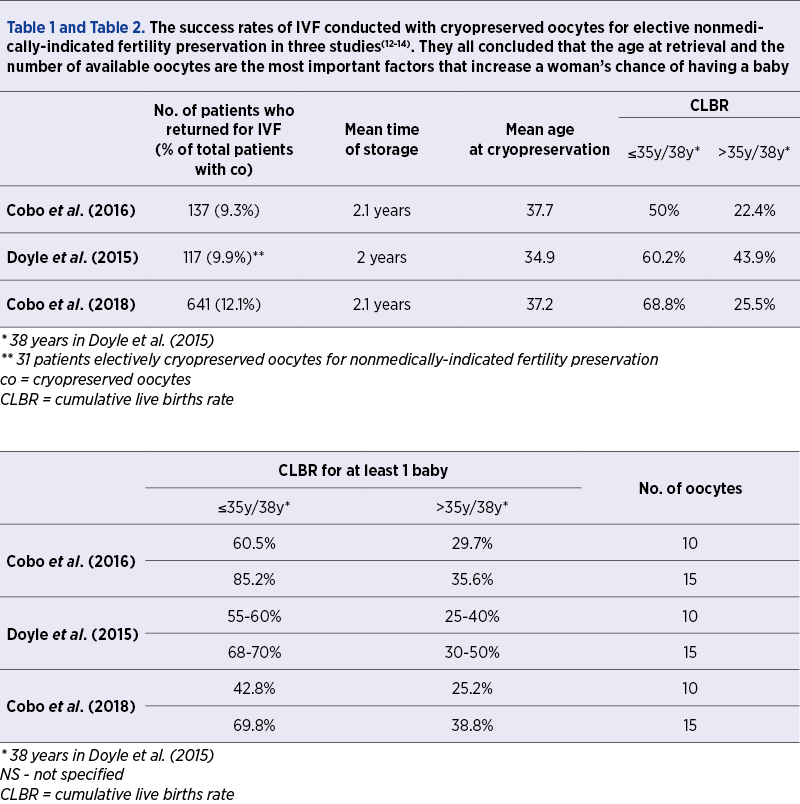
Cobo et al.(13) reported that the age at retrieval and the number of oocytes are the main factors that influence the success rate of achieving a pregnancy. The study showed that women ≤35 years old who used 10 mature oocytes had twice the success rate to achieve a live birth (60.5%) than women ≥36 years old who used the same number of oocytes and had a 29.7% likelihood of live birth. Regarding the number of oocytes which needed to be cryopreserved, they concluded that at least 8-10 metaphase II (MII) oocytes should be vitrified to obtain a reasonable success rate. Additionally, the cumulative live birth rate (CLBR) was higher and increased faster in younger women. The CLBR of women <35 years old raised from 15.4% for five oocytes to 40.8% for eight oocytes, reaching a plateau of 85.2% above 15 oocytes. For women older than 36 years old, the increase in CLBR was slower from 5.1% to 19.9% for five and eight oocytes, respectively. The CLBR plateau for this group was reached with 11 oocytes (35.6%).
Doyle et al.(14) compared the outcomes of IVF with both fresh and frozen oocytes to assess the likelihood of live birth per each oocyte depending on the age of the patient at retrieval. They suggested that 15-20 MII oocytes should be cryopreserved for women aged <38 years old (with approximately 70-80% chance of at least one live birth) and 25-30 MII oocytes for women aged 38-40 years old (with approximately 65-75% chance of at least one live birth). They found that women under 38 years old at oocyte retrieval have better chances of achieving a pregnancy than those over 38 years old (60.2% compared with 43.9%, respectively).
This study also concluded that using warmed vitrified oocytes has similar outcomes as using fresh oocytes, proving that oocytes cryopreservation is an effective method and confirming what other studies already revealed(8,9).
The study of Cobo et al.(12) is the largest study published to date and presents the outcomes of IVF cycles of 641 patients who cryopreserved oocytes for elective fertility preservation purposes. According to this study, women aged under 35 years old who cryopreserved 8-10 oocytes have a CLBR of approximately 30% and 45%, respectively. Furthermore, with 15 oocytes, the success rate can reach 70%. On the other hand, older patients (>35 years old) need more oocytes to achieve the same chances of having a baby as younger women, but the CLBR plateau is reached much earlier (50%). The CLBR of patients aged ≤35 year old was 68.8%, while the CLBR of patients aged >35 year was 25.5%. They emphasize the fact that the most important factor that impacts the success rate of IVF is the age at retrieval, proposing that, ideally, women should cryopreserve oocytes when aged ≤35 years old. Moreover, improved outcomes are reached when a higher number of oocytes are available, 10-15 oocytes being an indicated number.
Cost-efficiency
From a biological point of view, it is clear that the earlier a woman cryopreserves oocytes, the more chances she has for a successful IVF at the moment she decides to have children. However, these oocytes are less likely to be needed when women cryopreserve at very young ages, because they have a high probability of spontaneously conceiving a pregnancy. To determine the optimal timing for elective oocytes cryopreservation, one must balance the costs and benefits of this procedure.
Devin et al.(15) designed a model to determine whether cryopreserving oocytes at the age of 35 years old with the intention of using them for IVF at the age of 40 is more cost-effective than attempting pregnancy and, if needed, undergoing conventional IVF at the age of 40 years old. They concluded that oocyte cryopreservation before 38 years of age reduces the cost to obtain a live birth. Moreover, oocyte cryopreservation at the age of 35 years old in women intending to delay pregnancy until 40 years old would decrease the cost per live birth from around $55,000 to roughly $40,000 (with the likelihood of live birth increasing from 42% to 62%).
Another model(16) analyzed the optimal timing for cryopreserving oocytes from the cost-efficiency point of view. They found that performing oocyte cryopreservation at ages <34 years old ensures the highest probability of live birth (>74%). Instead, cryopreserving at the age of 37 years old compared to taking no action offers women the best chances of having a baby while being also the most cost-effective.
Van Loendersloot et al. demonstrated that, for a woman deciding to have a child at the age of 40 years old, cryopreserving oocytes at the age of 35 is the most cost-effective solution. They took into account three strategies: strategy 1 – women cryopreserve oocytes at the age of 35 and then at the age of 40 use these oocytes; strategy 2 – women at the age of 40 years old try to conceive without treatment; strategy 3 – women at the age of 40 years old attempt to conceive and, if not pregnant after one year, undergo IVF using freshly obtained oocytes. The results were as follows: strategy 1 had a live birth rate of 84.5% at an average cost of € 10,419; strategy 2 had a live birth rate of 52.3% at an average cost of € 310 per birth; strategy 3 had a live birth rate of 64.6% (31.4% after IVF and 33.2% after natural conception) at an average cost of € 7798. As they concluded in determining the success and cost-effectiveness of oocyte cryopreservation, the best results were achieved with strategy 1.
We can observe that a dilemma is emerging when considering the ideal age of cryoperserving oocytes. On one hand, biologically, the ideal age of cryopreserving is <35 years old and, on the other hand, the majority of studies show that elective fertility preservation is more cost-effective at 37-38 years old. Taking this into account but considering also that the chances of having a baby decrease when women vitrify at 36 years old or over, Cobo et al.(17) advise women to cryopreserve at the age < 36 years old. The Australasian ANZSREI consensus recommends that the best age to undertake oocyte cryopreservation is before 36 years old, although this would not be as cost-efficient as cryopreservation at the age of 37 years old. They state that at a younger age oocytes are of higher quality and of a greater number, which increases the likelihood of a live birth(1).
Obstetrical considerations
Elective cryopreservation of oocytes offers the opportunity to expand the reproductive lifespan of women, meaning that women who defer childbearing will become pregnant at a later age. We cannot disregard the remaining complications associated with pregnancy at an advanced maternal age (defined as >35 years old). When counseling women who take into consideration postponing motherhood, they should be informed about these risks. Advanced maternal age presents risks such as gestational diabetes, fetal growth restriction, preterm birth, labor complications and operative delivery. Additionally, women over the age of 40 have a higher prevalence of hypertensive disorders of pregnancy and almost twice the risk of developing preeclampsia(2,18). Nevertheless, these risks are the same as those in older women using conventional IVF(19).
The American Society for Reproductive Medicine committee advises that woman over 45 years old considering IVF with donor oocytes should be counseled regarding the obstetrical risks, the state of health of both parents, the physical and emotional challenges of raising a child, the possible impact on the child of having older parents, and the possibility of parental death before the child reaches adulthood(20). The same counseling should be given to women who are considering to cryopreserve oocytes and use them at an advanced age(18).
Conclusions
In today’s society, women are driven to postpone motherhood at the expense of losing their reproductive capacity. Oocyte cryopreservation provides the opportunity to extend fertility beyond a woman’s natural reproductive lifespan. In comparison with IVF, with donor oocyte vitrifying, their oocytes give the woman the possibility to have genetically linked children. With these new emerging topics and increasing interest toward it, healthcare providers have the responsibility to counsel women about the optimal time, success rates, the number of cryopreserved oocytes sufficient to achieve live birth and financial costs of cryopreservation, but also about the health risks arising with an advanced maternal age. It is important not to raise false hopes, especially because these women are undergoing a medical procedure only as a form of insurance against future declines in their fertility potential. The message of ESHRE remains that women should be primarily advised that the best chance of having a child is through natural reproduction at a relatively early age. They emphasize the need for official protocols to regulate elective oocyte cryopreservation(11). However, for women who do not have the option of naturally conceiving and wish to delay childbearing, oocytes cryopreservation offers a reasonable alternative.
Bibliografie
-
1. Lew R, Foo J, Kroon B, Boothroyd C, Chapman M, Australasian CREI Consensus Expert Panel on Trial evidence (ACCEPT) Group. ANZSREI consensus statement on elective oocyte cryopreservation. Aust NZJ Obstet Gynaecol. 2019 Oct; 59(5):616–626. doi: 10.1111/ajo.13028.
-
2. Jones BP, Saso S, Mania A, Smith JR, Serhal P, Nagi JB. The dawn of a new ice age: social egg freezing. Acta Obstet Gynecol Scand. 2018 Jun; 97(6):641–647. doi: 10.1111/aogs.13335.
-
3. American College of Obstetricians and Gynecologists Committee on Gynecologic Practice and Practice Committee. Female age-related fertility decline. Comitee Opinion no. 589. Fertil Steril. 2014 Mar;101(3):633–634. doi: 10.1016/j.fertnstert.2013.12.032.
-
4. Andersen A-MN. Maternal age and fetal loss: population based register linkage study. BMJ. 2000 Jun; 320(7251):1708–1712. doi: 10.1136/bmj.320.7251.1708.
-
5. van Loendersloot LL, Moolenaar LM, Mol BWJ, Repping S, van der Veen F, Goddijn M. Expanding reproductive lifespan: a cost-effectiveness study on oocyte freezing. Hum Reprod Oxf Engl. 2011 Nov; 26(11):3054–3060. doi: 10.1093/humrep/der284.
-
6. Habbema JDF, Eijkemans MJC, Leridon H, te Velde ER. Realizing a desired family size: when should couples start?. Hum Reprod. 2015 Sep;30(9):2215–2221. doi: 10.1093/humrep/dev148.
-
7. Sole M, et al. How does vitrification affect oocyte viability in oocyte donation cycles? A prospective study to compare outcomes achieved with fresh versus vitrified sibling oocytes. Hum Reprod. 2013 Aug;28(8):2087–2092. doi: 10.1093/humrep/det242.
-
8. Trokoudes KM, Pavlides C, Zhang X. Comparison outcome of fresh and vitrified donor oocytes in an egg-sharing donation program. Fertil Steril. 2011 May;95(6):1996–2000. doi: 10.1016/j.fertnstert.2011.02.035.
-
9. Cobo A, Meseguer M, Remohi J, Pellicer A. Use of cryo-banked oocytes in an ovum donation programme: a prospective, randomized, controlled, clinical trial. Hum Reprod. 2010 Sep;25(9):2239–2246. doi: 10.1093/humrep/deq146.
-
10. Practice Committees of the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology. Mature oocyte cryopreservation: a guideline. Fertil Steril. 2013 Jan;99(1):37–43. doi: 10.1016/j.fertnstert.2012.09.028.
-
11. ESHRE Task Force on Ethics and Law, including et al. Oocyte cryopreservation for age-related fertility loss. Hum Reprod. 2012 May;27(5):1231–1237. doi: 10.1093/humrep/des029.
-
12. Cobo A, García-Velasco J, Domingo J, Pellicer A, Remohí J. Elective and onco-fertility preservation: factors related to IVF outcomes. Hum Reprod. 2018 Dec;33(12):2222–2231. doi: 10.1093/humrep/dey321.
-
13. Cobo A, García-Velasco JA, Coello A, Domingo J, Pellicer A, Remohí J. Oocyte vitrification as an efficient option for elective fertility preservation. Fertil Steril. 2016 Mar;105(3):755-764.e8. doi: 10.1016/j.fertnstert.2015.11.027.
-
14. Doyle JO, Richter KS, Lim J, Stillman RJ, Graham JR, Tucker MJ. Successful elective and medically indicated oocyte vitrification and warming for autologous in vitro fertilization, with predicted birth probabilities for fertility preservation according to number of cryopreserved oocytes and age at retrieval. Fertil Steril. 2016 Feb;105(2):459-466. doi: 10.1016/j.fertnstert.2015.10.026.
-
15. Devine K, et al. Baby budgeting: oocyte cryopreservation in women delaying reproduction can reduce cost per live birth. Fertil Steril. 2015 Jun;103(6):1446-1453. doi: 10.1016/j.fertnstert.2015.02.029.
-
16. Mesen TB, Mersereau JE, Kane JB, Steiner AZ. Optimal timing for elective egg freezing. Fertil Steril. 2015 Jun;103(6):1551-1556.e1–4. doi: 10.1016/j.fertnstert.2015.03.002.
-
17. Cobo A, García-Velasco JA. Why all women should freeze their eggs. Curr Opin Obstet Gynecol. 2016 Jun;28(3):206–210. doi: 10.1097/GCO.0000000000000269.
-
18. Bachmann G, MacArthur TA, Khanuja K. Need for Comprehensive Counseling in Women Requesting Oocyte Cryopreservation. J Womens Health. 2018 Mar;27(3):227–230. doi: 10.1089/jwh.2017.6423.
-
19. Goold I, Săvulescu J. In favour of freezing eggs for non-medical reasons. Bioethics. 2000 Jan;23(1):47–58. doi: 10.1111/j.1467-8519.2008.00679.x.
-
20. Daar J, et al. Oocyte or embryo donation to women of advanced reproductive age: an Ethics Committee opinion. Fertil Steril. 2016 Oct;106(5):pp. e3–e7. doi: 10.1016/j.fertnstert.2016.07.002.