Clubfoot represents a congenital limb deformity, with a frequency of 1/1000 pregnancies, and it is one of the most common musculoskeletal deformities presenting at birth. Although it is diagnosed at birth, many cases are detected from the antenatal period, following an ultrasound examination. In about half of the cases, both feet are affected, boys being twice more likely than girls to have the deformity. Objective. This study aims to review the literature regarding the outcome of isolated clubfoot and the risk that stems from its association with other anomalies. Materials and method. The online database was used to detect studies that have evaluated the outcome of isolated clubfoot or associated with other abnormalities. The information from literature was compared with our experience at the Antenatal Diagnostic Unit from the Emergency County Clinical Hospital of Craiova, based on the ultrasound assessments performed during 2018. Results. If the malformation is isolated, it will have a good prognosis. It may be postural, especially in pelvic presentations associated with a reduced amniotic fluid. In complex clubfoot cases, associated with other structural abnormalities, a chromosomal abnormality may be diagnosed, or the cause may be neurological or muscular, and it is part of a syndrome. Conclusions. Because of the significant different prognosis, it is important to carry out an antenatal ultrasound diagnosis, as complex as possible, to discriminate between the presence of an isolated clubfoot from the cases where this abnormality is associated with other malformations.
Rezultatele privind diagnosticarea prenatală a piciorului strâmb congenital izolat sau complex – review sistematic şi serie de cazuri
Outcome in prenatal diagnosis of isolated or complex clubfoot – systematic review and case series
First published: 29 octombrie 2019
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/ObsGin.67.3.2019.2614
Abstract
Rezumat
Piciorul strâmb congenital, una dintre cel mai des întâlnite deformări congenitale ale membrelor, cu o frecvenţă de 1/1000 de sarcini, este una dintre cele mai frecvente malformaţii musculoscheletale prezente la naştere. Deşi afecţiunea este diagnosticată la naştere, multe cazuri sunt detectate încă din perioada antenatală, în urma unui examen ecografic. În aproximativ jumătate dintre cazuri, ambele picioare sunt afectate, băieţii fiind de două ori mai predispuşi decât fetele. Obiectiv. Scopul a fost de a realiza un review al literaturii de specialitate în vederea stabilirii prognosticului în cazul diagnosticării piciorului strâmb congenital izolat, dar şi în cazul asocierii lui cu alte anomalii. Materiale şi metodă. Am utilizat baza de date online pentru a detecta studii ce au evaluat prognosticul în cazul diagnosticării piciorului strâmb congenital izolat, dar şi asociat cu alte anomalii. Review-ul sistematic se bazează pe eforturile de a găsi cele mai bune studii posibile care să răspundă la întrebarea noastră. Datele din literatură au fost completate cu date obţinute din evaluările ecografice efectuate pe o perioadă de un an (2018) în cadrul Unităţii de diagnostic antenatal din cadrul Spitalului Clinic Judeţean de Urgenţă din Craiova. Rezultate. Dacă malformaţia este izolată, are un prognostic bun. Ea poate fi posturală, mai ales în prezentaţiile pelviene asociate cu o cantitate redusă de lichid amniotic. În formele complexe, asociate cu alte anomalii structurale, cauza poate fi neurologică sau musculară şi este parte dintr-un sindrom sau este diagnosticată o anomalie cromozomială. Concluzii. Este importantă realizarea unui diagnostic antenatal ecografic cât mai complex, care să diferenţieze prezenţa piciorului strâmb congenital izolat de cazurile în care această modificare este prezentă alături de alte anomalii.
Introduction
The clubfoot has a frequency of 1/1000 pregnancies and it is one of the most common congenital malformations involving the musculoskeletal system. Ultrasonographically, there are several aspects of the congenital clubfoot. The foot is fixed with three distinct abnormalities present: hindfoot equinus and varus, midfood supination and forefoot adductus(1). T.W. Hester et al.(2) realized a literature research and proposed that the underlying unifying factor in all cases of clubfoot is a lack of fetal movement. Fetal movement is important for the development of joints, and they suggested that this applies to the morphogenesis of the forefoot. On ultrasound, the varus equin foot is diagnosed by visualizing the tibia and fibula in the same longitudinal plane as the lateral aspect of the foot. The appearance of varus equin is normal up to 12 weeks of pregnancy. Although the congenital clubfoot can be prenatally suspected from the first trimester of pregnancy, the diagnosis is established after birth. Two classification systems are widely used in the initial assessment of clubfoot deformations. One of these classification systems was developed by Dimeglio, and the second by Pirani. Both systems apply a score based on a number of different physical findings which, when totalized, lead to a value that correlates with the severity of the foot injury.
The widespread use of ultrasound during pregnancy and the improved techniques had greatly increased the diagnosis rate of anomalies, including musculoskeletal malformations.
The main purpose of this review is to provide information on the outcome of isolated or complex clubfoot.
Materials and method
We assumed an objective attitude towards updated information. To answer to our question – the outcome of isolated or complex clubfoot – we used comparable studies published between 1998 and 2018, which were identified via PubMed search, using the keywords: outcome clubfoot, antenatal clubfoot, isolated clubfoot, complex clubfoot. The studies were included based on providing prenatal and postnatal data. Also, we used the data obtained from the ultrasound assessments performed at the Antenatal Diagnostic Unit from the Emergency Clinical County Hospital of Craiova. Eight articles from our search met the inclusion criteria (Table 1).
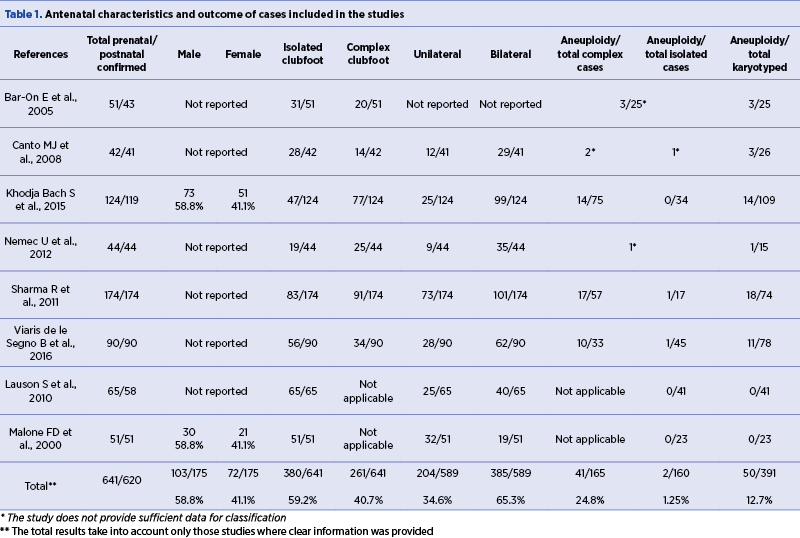
In a study of 124 cases, S. Khodja Bach et al.(3) investigated the opportunity to perform invasive genetic maneuvers in cases of isolated clubfoot. They did not find any chromosomal abnormalities in cases of idiopathic or isolated talipes equinovarus. The study results showed that amniocentesis should not be applied systematically in isolated talipes equinovarus (TEV) cases, with a familial history of clubfoot and a male fetus. However, in all cases it is recommended that a referent echographist in prenatal diagnosis should perform a morphologic echography.
U. Nemec et al.(4) tried to identify the role of MRI evaluation of fetuses with talipes equinovarus. This retrospective study included the MRI scans of 44 fetuses. Ultrasound reports were available for comparison in 42/44 cases. The comparison of the MRI findings and of the previous ultrasound findings showed that fetal MRI enables differentiation between isolated and complex talipes equinovarus and there are no further findings when the ultrasound diagnosis isolated TEV. Additional MRI findings were confirmed in 8/42 (19.0%) cases, seven of which were related to brain and spine anomalies. Fifteen of the 44 fetuses underwent karyotyping from which one had trisomy 18.
P. Stone(5) and collaborators analyzed the long-term outcomes in 163 children at school age diagnosed with isolated idiopathic congenital talipes equinovarus (CTEV) at birth. They found a rate of additional abnormalities higher than previously reported, of 30.1%. Regarding the spectrum of the abnormalities, 41% were associated with the central nervous system or neurodevelopmental delay. Although conventional G-band karyotyping was performed, this investigation did not reveal supplementary information, thus the authors concluded that karyotyping in cases of unilateral or bilateral talipes equinovarus is unlikely to detect chromosomal abnormalities.
A study from D.R. Hartge and collaborators(6) (2012) on 106 children with unilateral or bilateral CTEV detected prenatally in a period of 17 years concluded that the prognosis of children with isolated clubfoot is good, but in the complex cases the outcome depends on the association of additional structural and genetic anomalies, thus fetal karyotyping is mandatory in such cases.
S. Lauson et al.(1) analyzed the aneuploidy risk and treatment outcome in 65 cases prenatally diagnosed with isolated clubfoot. Aneuploidies were not identified by cytogenetic analysis or clinical assessment in the study group. Considering the studies published between 1996 and 2008, they calculated the risk of aneuploidy associated with the ultrasound finding of isolated clubfoot as 1.7%, based on clinical assessment or karyotype analysis, or 3.6% if considering only the karyotyped patients.
R. Sharma et al.(7) conducted a retrospective observational study on the perinatal outcome of prenatally diagnosed congenital talipes equinovarus in 174 cases. They concluded that the perinatal outcome is poor when others abnormalities are associated. The perinatal mortality rate in this group was significantly higher (64.8%) compared with the isolated group (1.2%). The risk of aneuploidy was increased if there were additional structural abnormalities present. The aneuploidy rate was 30% in the non-isolated group compared with 1.2% in the isolated one.
In another study with a similar design, D. Fergal Malone et al.(8) found that karyotyping should not be offered when isolated unilateral or bilateral clubfoot is prenatally diagnosed. In all 51 cases of isolated clubfoot there were no cases of fetal aneuploidy on fetal karyotype evaluation or newborn physical examination. However, the study emphasized the need of a detailed sonographic fetal anatomy survey to rule out additional abnormalities.
Deborah Krakow(9) reported that genetic disorders or chromosomal abnormalities were rarely confirmed in association with isolated clubfoot. This contrasts with clenched hands, which rarely present as isolated anomalies.
B. Viaris de le Segno et al.(10) confirmed that fetal karyotyping is required in cases of complex clubfoot because of the increased rate of aneuploidy and adverse pregnancy outcomes, while the need for invasive diagnostic in isolated clubfoot remains controversial.
In a study in which clubfoot was diagnosed by ultrasonography in 52 fetuses, E. Bar-On et al.(11) performed karyotyping in 25 cases and noticed abnormalities in three complex clubfoot fetuses.
T.D. Shipp et al.(12) (1998) recommended invasive diagnostic in isolated clubfoot cases because other malformations may not be detected ultrasonographically in the early second trimester. However, modern ultrasound equipment have helped to improve the diagnosis in early pregnancy.
Another retrospective study of 20,663 pregnant women found that one-third of the fetuses prenatally diagnosed with clubfoot were cases with complex malformation. The risk of requiring surgery was about 40% for isolated clubfoot, and the detection of a bilateral defect did not worsen the prognosis(13).
In our retrospective observational series of cases we included all patients with prenatally diagnosed isolated or complex clubfoot seen during 2018, at the Antenatal Diagnostic Unit from the County Emergency Clinical Hospital of Craiova. We identified a total of 12 cases with prenatally isolated and complex clubfoot. Five of them were associated with other anomalies and seven were isolated. From the isolated cases, one was false positive. Of the six remained cases of isolated talipes, four were unilateral (with equal right and left distribution) and two were bilateral. Of the five cases of talipes associated with additional anomalies, three were reported as unilateral and two were bilateral (Table 2). The commonest associated structural abnormalities were brain (two cases) and heart malformations (three cases).
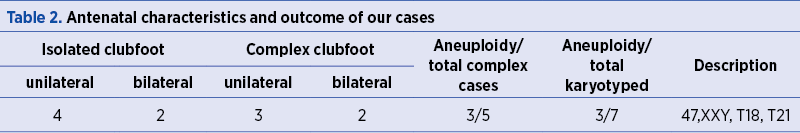
We performed karyotype for four patients with isolated clubfoot and none of them had aneuploidy identified by cytogenetic analysis. In the group of complex clubfoot we managed to perform karyotype in three cases and all of them had aneuploidy, respectively 47XXY, T18 and T21.
Case report
A 28-year-old primigesta woman was referred to our clinic at the County Emergency Clinical Hospital of Craiova for a third-trimester ultrasound evaluation. She had no previous pregnancy scans and she was diagnosed with gestational diabetes in late second trimester. During the scan, it has been noticed the presence of associated anomalies, varying from minor to major degree: severe facial defect with cleft lip and palate, flattened facial profile, hypertrophic umbilical cord with cystic aspect, membranous ventricular septal defect, hydronephrosis, brachycephaly, cerebellar hypoplasia, clenched hands and unilateral clubfoot. The sonographic aspects of the abnormalities are presented in Figure 1 and Figure 2.
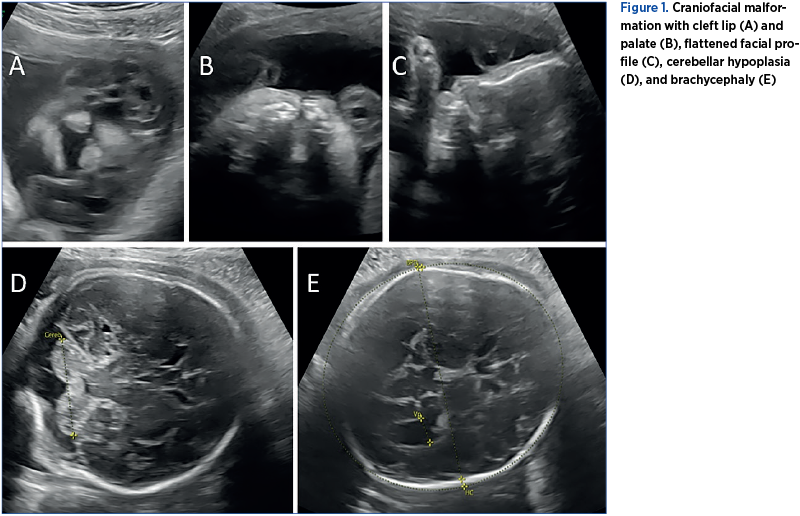
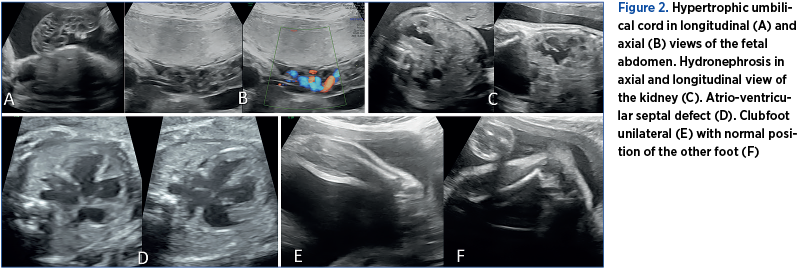
The patient was counseled that the birth should take place in a tertiary center. A premature baby boy of 2000 g was born by vaginal delivery. The neonatologist and pediatric surgeon confirmed the presence of left facial (lip and palate) defect, left club foot, lower and upper limb arthrogryposis, and bilateral cryptorchidism. The cardiologist confirmed a large perimembranous septal defect. The baby died at 12 days old due to cardiorespiratory arrest. All sonographic and postnatal findings were confirmed by anatomopathological examination. At birth, a blood sampling was tested by our Human Genetics Laboratory, with a result for an abnormal fetal karyotype – trisomy 18. The couple was also genetically tested and the results revealed normal karyotype for both of them.

Discussion
Out of 641 cases of isolated and complex clubfoot from the studies we reviewed, there were 620 follow-ups. The global sex ratio shows that the boys are almost twice more likely than girls to have the deformity. Of the 641 patients prenatally diagnosed with clubfoot, 380 (59.2%) were diagnosed as isolated and 261 (40.7%) as complex. With regard to laterality, the defect was unilateral in 204 (34.6%) and bilateral in 385 (65.3%) out of the affected fetuses. Of the 641 patients, 391 had cytogenetic analysis done on either amniocytes or postnatal blood samples. Fifty of them had abnormal karyotype (12.7%), two of the cases being isolated and 41 cases being complex clubfoot. Combining the results from these studies, the aneuploidy risk for isolated clubfoot is 1.25% based on isolated cases which have been karyotyped. On the contrary, the risk that the fetus has a chromosomal abnormality is higher, 24.8%, when we refer to complex clubfoot.
In our small series we noticed that complex clubfoot has a poor outcome when it is associated with other structural anomalies. Furthermore, in this situation, it is very likely that the fetus has a chromosomopathy, fetal karyotyping being required in cases of complex clubfoot.
After analyzing all the studies included in our review, we can support the idea that in case of isolated clubfoot, chromosomal abnormalities were sporadically present and the outcome was good. On the other hand, in complex clubfoot, the outcome depends on the additional anomalies the fetus has. Also, another conclusion is that there are a poor perinatal outcome and an increased risk of aneuploidy when other abnormalities are associated or in case of prenatally diagnosed cases of complex clubfoot.
In terms of the invasive prenatal testing, there is one study which recommended karyotyping evaluation when isolated clubfoot is identified because associated malformations may not be detected ultrasonographically(12). However, it was published several decades ago, and the resolution of modern ultrasound equipment, along with the development of training programs in prenatal diagnosis allow nowadays for a much more precise fetal structural investigation.
The prenatal diagnosis of isolated clubfoot should always include an appropriate prenatal counseling together with pediatric orthopedics and pediatric surgeons, and there is mandatory to repeat ultrasound scans to reduce the risk of misjudgment of additional fetal anomalies as those may be frequently seen in these fetuses. Moreover, serial ultrasound examinations are helpful to decrease the false positive diagnosis. Literature suggests that when counseling women regarding prenatally diagnosed isolated clubfoot, it is important to inform them that approximately 10% of individuals will have a normal foot or positional foot deformity requiring minimal treatment. Conversely, 10-13% of prenatally diagnosed cases of isolated clubfoot will have complex clubfoot postnatal, with additional structural or neurodevelopmental abnormalities.
Because there is an increasing incidence of antenatal detection of associated anomalies, it is suggested that parents require adequate antenatal counseling by a specialist in the area of clubfoot. The information should improve both the orthopedic surgeons and parents in terms of understanding the natural history and treatment of this condition(14,15). Also, due to the fact that clubfoot prenatal detection is higher when the condition is bilateral and/or other anomalies are associated, it is important that parents be informed that, in suspected isolated talipes, some associated anomalies might remain undetected prenatally(16).
Despite the significant improvements in obstetric ultrasound, which have led to an increased prenatal detection of clubfoot, studies have not been able to correlate the sonographic appearance with the severity of clinical deformity birth. M.P. Glotzbecker and colab. developed a novel sonographic scoring system which showed improved detection of a true clubfoot prenatally and a decrease in the false-positive rate. This algorithm takes into account the angle that the long-axis of the foot made with the long-axis of the lower leg. The categories were defined as: Normal – when there is no angle between the long axis of the lower leg and long axis of the foot; Mild – greater than 0 and less than or equal to 80 degree angle between the long axis of the lower leg and long axis of the foot; Moderate – greater than 80 and less than or equal to 100 degree angle; Severe – greater than 100 degree angle. According to the respective scoring system, an isolated “mild” clubfoot case diagnosed prenatally is less likely to end up as a clubfoot at birth. This finding will have substantial impact on prenatal counseling(17).
Our results are in line with the overall results of previous studies. There is a limitation of our study and of previous researches as well, since we have no data on whether all the fetuses who did not have karyotype evaluations were truly chromosomally normal. By combining our results with those previously published, patients should be counseled that the prenatal finding of isolated clubfoot is associated with a low risk of chromosomal abnormalities and with an overall good outcome. Additionally, in complex clubfoot, the outcome depends on the additional anomalies that are present.
Regarding the case presented before, although the fetus presented unilateral clubfoot, severe anomalies were associated in the context of trisomy 18 chromosomopathy: cerebral, urinary, craniofacial and cardiovascular. Therefore, professionals should be aware that, even rarely, isolated clubfoot may be associated with major structural and/or chromosomal abnormalities. The case also presented another particularity, the association with gestational diabetes. It was found that women with gestational diabetes may have a higher relative risk of 7.7 to have an infant with a numeric sex chromosome defect, perhaps due to underlying biochemical changes that induce non-disjunction and the development of chromosomal defects(18). On the other hand, the malformations risk increases linearly with the degree of maternal hyperglycemia, which is a major teratogenic factor, and determine up to a nine-fold increase in congenital malformations, compared with the non-diabetic pregnancies(19). The pathophysiological mechanism is complex and includes increased oxidative stress and altered gene expression. Oxidative stress activates cellular stress signaling, dysregulation in gene expression and excess apoptosis, while alteration of the gene expression causes deviation from the normal structural development. Most of the malformations in diabetic pregnancies are related to the cardiovascular, central nervous and musculoskeletal systems, as presented in our case(20-22). These facts underline the importance of early detailed morphological evaluation of fetuses in diabetic pregnancies(23).
Conclusions
Isolated clubfoot represents a fetal congenital malformation with a good prognosis. It may be postural, especially in pelvic presentations associated with reduced amniotic fluid. In bilateral or complex cases, associated with other structural abnormalities, a chromosomal abnormality may be diagnosed, or the cause may be neurological or muscular and it is part of a syndrome. It seems important to carry out a detailed antenatal ultrasound examination, as complex as possible, to distinguish the presence of an isolated clubfoot from the cases where this malformation associates other abnormalities. Amniocentesis should not be applied systematically in isolated clubfoot cases. However, fetal karyotyping is mandatory in complex clubfoot cases, as the outcome depends on the associated structural or genetic abnormalities.
This review is important because it provides contemporary data that can be used to counsel women prenatally. Prenatal counseling should be offered to parents with affected fetuses together with pediatric orthopedics and pediatric surgeons.
It is difficult to counsel parents regarding the chances for a false-positive talipes diagnosis, but serial prenatal scans are helpful to discriminate more accurately the affected fetuses, and to reduce the risk of misjudgment of additional fetal anomalies.
Disclosure: Authors declare no conflicts of interest. They do not have interests which may be perceived as posing a conflict or bias. They have no financial interests in any company or organization that might benefit from the publication.
Bibliografie
1. Lauson S, Alvarez C, Patel MS, Langlois S. Outcome of prenatally diagnosed isolated clubfoot. Ultrasound Obstet Gynecol. 2010 Jun; 35(6):708-14. doi: 10.1002/uog.7558.
2. Hester TW, Parkinson LC, Robson J, Misra S, Sangha H, Martin JE. A hypothesis and model of reduced fetal movement as a common pathogenetic mechanism in clubfoot. Med Hypotheses. 2009 Dec; 73(6):986-8. doi: 10.1016/j.mehy.2009.04.056. Epub 2009 Sep 27.
3. Khodja Bach S, Houfflin-Debarge V, Vaast P, Wapler C, Coulon C. Clubfoot’s prenatal ultrasound diagnosis: is amniocentesis always warranted? About 124 cases. Gynecol Obstet Fertil. 2015 Feb; 43(2):117-22. doi: 10.1016/j.gyobfe.2014.12.001. Epub 2015 Jan 27.
4. Nemec U, Nemec SF, Kasprian G, Brugger PC, Bettelheim D, Wadhawan I, Kolb A, Graham JM Jr, Rimoin DL, Prayer D. Clubfeet and associated abnormalities on fetal magnetic resonance imaging. Prenat Diagn. 2012 Sep; 32(9):822-8. doi: 10.1002/pd.3911. Epub 2012 Jun 8.
5. Stone P, Martis W, Crawford H. Idiopathic congenital talipes equinovarus; not always an isolated anomaly. A review of long-term outcomes. J Matern Fetal Neonatal Med. 2018 Oct; 31(20):2693-2698. doi: 10.1080/14767058.2017.1353967. Epub 2017 Jul 20.
6. Hartge DR, Gaertner S, Weichert J. Prenatal detection and postnatal outcome of congenital talipes equinovarus in 106 fetuses. Arch Gynecol Obstet. 2012 Oct; 286(4):831-42. doi: 10.1007/s00404-012-2325-3. Epub 2012 May 13.
7. Sharma R, Stone S, Alzouebi A, Hamoda H, Kumar S. Perinatal outcome of prenatally diagnosed congenital talipes equinovarus. Prenat Diagn. 2011 Feb; 31(2):142-5. doi: 10.1002/pd.2655. Epub 2011 Jan 3.
8. Malone FD, Marino T, Bianchi DW, Johnston K, D’Alton ME. Isolated clubfoot diagnosed prenatally: is karyotyping indicated? Obstet Gynecol. 2000 Mar; 95(3):437-40.
9. Krakow D. Obstetric Imaging. Fetal Diagnosis and Care. 2018; pp.305-308.e1.
10. Viaris de le Segno B, Gruchy N, Bronfen C, Dolley P, Leporrier N, Creveuil C, Benoist G. Prenatal diagnosis of clubfoot: Chromosomal abnormalities associated with fetal defects and outcome in a tertiary center. J Clin Ultrasound. 2016 Feb; 44(2):100-5. doi: 10.1002/jcu.22275. Epub 2015 Jul 14.
11. Bar-On E, Mashiach R, Inbar O, Weigl D, Katz K, Meizner I. Prenatal ultrasound diagnosis of club foot: outcome and recommendations for counselling and follow-up. J Bone Joint Surg Br. 2005 Jul; 87(7):990-3.
12. Shipp TD, Benacerraf BR. The significance of prenatally identified isolated clubfoot: is amniocentesis indicated? Am J Obstet Gynecol. 1998 Mar; 178(3):600-2.
13. Canto MJ, Cano S, Palau J, Ojeda F. Prenatal diagnosis of clubfoot in low-risk population: associated anomalies and long-term outcome. Prenat Diagn. 2008 Apr; 28(4):343-6. doi: 10.1002/pd.1984.
14. Burgan HE, Furness ME, Foster BK. Prenatal ultrasound diagnosis of clubfoot. J Pediatr Orthop. 1999 Jan-Feb; 19(1):11-3.
15. Treadwell MC, Stanitski CL, King M. Prenatal sonographic diagnosis of clubfoot: implications for patient counseling. J Pediatr Orthop. 1999 Jan-Feb; 19(1):8-10.
16. Offerdal K, Jebens N, Blaas HG, Eik-Nes SH. Prenatal ultrasound detection of talipes equinovarus in a non-selected population of 49 314 deliveries in Norway. Ultrasound Obstet Gynecol. 2007 Nov; 30(6):838-44.
17. Glotzbecker MP, Estroff JA, Spencer SA, Bosley JC, Parad RB, Kasser JR, Mahan ST. Prenatally diagnosed clubfeet: comparing ultrasonographic severity with objective clinical outcomes. J Pediatr Orthop. 2010 Sep; 30(6):606-11. doi: 10.1097/BPO.0b013e3181e78e4e.
18. Moore LL, Bradlee ML, Singer MR, Kenneth KJ, Milunsky A. Chromosomal anomalies among the offspring of women with gestational diabetes. Am J Epidemiol. 2002 Apr 15; 155(8): 719–724.
19. Versiani BR, Gilbert-Barness E, Giuliani LR, Peres LC, Pina-Neto JM. Caudal dysplasia sequence: severe phenotype presenting in offspring of patients with gestational and pregestational diabetes. Clin Dysmorphol. 2004; 13:1–5.
20. Schaefer-Graf UM, Buchanan TA, Xiang A, Songster G, Montoro M, Kjos SL. Patterns of congenital anomalies and relationship to initial maternal fasting glucose levels in pregnancies complicated by type 2 and gestational diabetes. Am J Obstet Gynecol. 2000; 182:313–320.
21. Aberg A, Westbom L, Källén B. Congenital malformations among infants whose mothers had gestational diabetes or preexisting diabetes. Early Hum Dev. 2001; 61:85–95.
22. Yang J, Cummings EA, O’connell C, Jangaard K. Fetal and neonatal outcomes of diabetic pregnancies. Obstet Gynecol. 2006; 108:644–650.
23. Gheorman L, Iliescu D, Ceauşu I, Paulescu D, Pleşea IE, Gheorman V. Importance of early complex evaluation in high-risk pregnancy associated to diabetes mellitus. Case presentation and review of the literature. Rom J Morphol Embryol. 2011; 52(3 Suppl): 1127–1132.
Articole din ediţiile anterioare
Distanţa dintre vezicula vitelină şi embrion asociată cu inhibina A în sarcina de trimestrul I – care este noutatea?
Etiologia decesului embrionar este multifactorială, anomaliile cromozomiale fiind cele mai frecvente (40%). Scopul acestui studiu este de a evalua ...
Efectul apendicectomiei asupra rezultatelor sarcinii în curs. O investigaţie preliminară bazată pe chestionare
Scop. Am evaluat impactul apendicetomiei asupra prognosticului obstetrical al unei sarcini ulterioare. Materiale şi metodă. A fost realizat un stud...
Rezultatele obstetricale şi neonatale ale sarcinilor complicate de infecţia cu SARS-CoV-2
Pandemia de COVID-19 are un impact fără precedent. Femeile gravide fac parte din populaţia vulnerabilă, iar amploarea consecinţelor infecţiei cu SA...