Ketamine is an N-methyl-D-aspartate (NMDA)-receptor antagonist approved as an anesthetic agent in the USA that recently gained traction as an analgesic drug. In palliative care and pain medicine, ketamine is frequently used, mostly as an opioid sparing agent, for acute postoperative pain and for difficult-to-treat pain conditions. Ongoing clinical evidence supports ketamine’s analgesic role; however, prestigious organizations like the National Comprehensive Cancer Network (NCCN) and the European Society for Medical Oncology (ESMO) recommend the need for more research in this field. Ketamine acts on numerous receptors, which could explain both its analgesic effects and its numerous side effects, with psychotomimetic effects being the most disturbing to patients and the main reason for the discontinuation of therapy. Clinicians should carefully screen patients prior to initiating ketamine because of its side effects and potential for abuse.
Ketamina în doze mici în analgezie – o nouă abordare?
Low-dose ketamine in analgesia – a novel approach?
First published: 30 octombrie 2018
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/OnHe.44.3.2018.2023
Abstract
Rezumat
Ketamina, aprobată ca agent anestezic în Statele Unite ale Americii, acţionează ca un antagonist pe receptorii N-methyl-D-aspartat (NMDA), care influenţează toleranţa la opioide, dar şi hiperalgezia produsă de către opioide. Ketamina câştigă popularitate ca agent analgezic în medicina de îngrijire paliativă şi în medicina durerii, cu predominanţă în managementul durerii acute postchirurgicale şi pentru condiţiile dureroase cronice dificil de tratat. Numeroase studii demonstrează beneficiile utilizării ketaminei, dar organizaţii prestigioase ca NCCN şi ESMO sugerează că este necesară mai multă informaţie ştiinţifică înainte de a o îmbrăţişa ca agent analgezic. Efectele secundare psihiatrice ale ketaminei, care sunt cele mai îngrijorătoare pentru pacienţi, împreună cu riscul de abuz necesită o selecţie atentă a pacienţilor înainte de iniţierea terapiei cu ketamină.
Poorly managed pain, especially cancer pain, adversely affects patient outcomes, such as compliance with oncologic treatments, patient satisfaction with medical care, and prolonged hospital stays, with frequent readmissions for pain management. All of these factors increase healthcare costs.
Over 30 years ago, the World Health Organization (WHO) adopted the three-step analgesic ladder (Figure 1) to guide clinicians on how to appropriately and safely treat pain(1).
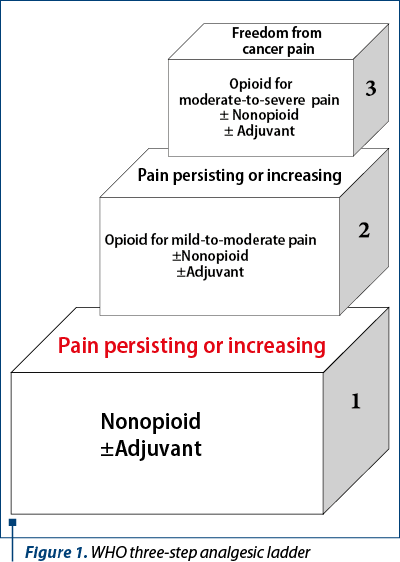
However, in patients with cancer and cancer treatment related pain, a two-step approach involving opioids may be more appropriate.
Yet, with the current misuse and abuse of opioids, which have led to the “opioid crisis” in the United States, more clinicians are considering other modalities to address cancer pain. There may be a role for ketamine here considering its potential to decrease opioid-induced hyperalgesia and decrease opioid requirements, while also having lower risk of adversely affecting hemodynamic function and respiratory drive compared to opioids(2).
Ketamine, known in the US as Ketalar, is listed as a schedule III-controlled substance and is an N-methyl-D-aspartate (NMDA)-receptor antagonist. It was synthesized by Parke Davis Pharmaceutical Company in 1962 and became known as a field anesthetic during the Vietnam War. It is currently approved by the US Food and Drug Administration as an anesthetic agent, but has gained popularity for its off-label use at sub-anesthetic doses for chronic pain management and the treatment of refractory depression(3).
NMDA receptors are involved in central sensitization, neural plasticity, opioid tolerance, and opioid-induced hyperalgesia. Ketamine binds to the phencyclidine (PCP) site of NMDA receptors, resulting in activation(4).
In addition to the NMDA receptors, ketamine also acts on a myriad of other receptors, including µ, d and k opioid receptors, nicotinic, muscarinic, dopamine and serotoninergic receptors, in addition to voltage-gated Na and K channels, which are responsible for its analgesic effect, but also for its numerous side effects(5,6).
Ketamine exists as a racemic mixture of R (−) and S (+) stereoisomers. The S (+) stereoisomer has a shorter duration of action, but is approximately three to four times more potent than the R (−) stereoisomer, possibly due to its greater affinity for the PCP site on the NMDA receptor(7).
Ketamine is indicated as a sedative agent, with off-label indications including sub-anesthetic doses for treatment-refractory depressive disorders, postoperatively as an opioid sparing agent, and for difficult-to-manage pain conditions. Palliative care and interventional pain management specialists are becoming increasingly familiar with the latter off-label indication for ketamine, which represents the focus of this article. Patients who could benefit from ketamine therapy, as a sole agent or in combination with opioids, are those suffering from complex regional pain syndrome (CRPS), painful persistent peripheral neuropathy, stump or phantom limb pain, severe postherpetic neuralgia, or refractory cancer pain. Studies suggest that young patients with short pain histories (less than 5 years) may benefit the most from the analgesic effects of ketamine(6).
Ketamine can be administered by multiple routes, such as oral (PO), nasal, rectal, topical, subcutaneous (SQ), intramuscular (IM), intravenous (IV), epidural or intrathecal(6).
When describing the routes of administration, the following points are important to note:
1. There are no commercially available oral forms and therefore patients are recommended to take compounded capsules or the injection fluid mixed with some fruit juice or cola to mask its bitter taste.
2. Intranasal administration uses an undiluted solution of 50 mg/ml or a solution diluted with normal saline to a concentration of 20 mg/ml.
3. The undiluted form of 50 mg/ml could be used rectally.
4. SQ administration could cause painful induration at the injection site.
5. Some studies found focal lymphocytic vasculitis close to the injection site with intrathecal administration possibly related to the preservatives benzethonium chloride or chlorobutanol, and therefore the preservative-free formulation is favored(5,6,8).
Ketamine can be used topically for localized or neuropathic pain in compounded cream preparations with ketamine 10% along with a combination of gabapentin 6% and/or clonidine 0.2% and/or baclofen 2% and/or imipramine 3% and/or nifedipine 2% and/or diclofenac 3% and/or lidocaine 5%. Patients need to apply the ketamine ointment only over the most painful areas on intact skin and not over the entire area of pain.
Several studies have shown that IV ketamine may decrease postoperative opioid consumption. Nielsen et al. found a significant decrease in IV morphine use in patients with chronic pain after spinal surgery who had received low-dose ketamine intraoperatively(9). In one article, Allen and Ivester reviewed 39 studies of ketamine use and identified an approximately 40% decrease in postoperative opioid consumption, suggesting a possible reduction in the risk of developing persistent postoperative pain. The postoperative infusion rates ranged between 0.002 mg/kg/hour to 0.2 mg/kg/hour(10).
Another study concluded that low-dose ketamine infusion should be included in the treatment plan for patients with chronic pain who are planning to have a surgical procedure based on their results which showed a 71% reduction in opioid consumption at the 6-week postoperative visit(2).
Boenigk et al. showed that postoperative administration of low-dose ketamine reduced opioid requirements for the first 24 hours following spinal fusion surgery in opioid-tolerant, but not in opioid-naïve patients(11).
Before utilizing IV or SQ ketamine for chronic difficult-to-treat conditions, clinicians need to screen patients for all possible contraindications, inform them of the potential side effects, get consent (if applicable), and place the patient on continuous telemetry and oxygen monitoring (if in accordance with the institutional policies).
Consent and continuous monitoring may not be necessary in palliative care settings, especially when patients have terminal cancer, are experiencing extreme suffering, or are receiving palliative sedation.
Two of the several protocols that have been proposed when using IV or SQ ketamine at sub-anesthetic doses are as follows:
I.
1. Administer a loading dose of 0.1-0.2 mg/kg intravenously or 0.5 mg/kg subcutaneously while monitoring pain scores and potential side effects.
2. Consider adding a benzodiazepine, an antipsychotic or an antisialagogue if dysphoria or sialorrhea occur.
3. Double the dose of ketamine if there is no change in pain score within 15 minutes of IV administration or within 30-45 minutes of SQ administration.
4. Repeat number 3 until pain relief is obtained.
5. Start a continuous infusion at an hourly rate at the dose that provided the patient with pain relief.
6. Consider decreasing opioid doses by 50% if pain control is obtained or if the patient is experiencing side effects from opioids.
7. Consider further decrease of opioids by an additional 50% every 24 hours as tolerated(12).
II.
1. Administer a loading dose of 0.25-0.5 mg/kg over 30 minutes while monitoring pain scores and potential side effects.
2. Consider administering boluses of 0.5 mg/kg if the patient has responded.
3. Consider increasing the boluses by 0.5 mg/kg until pain relief is obtained or the patient is experiencing side effects. The mean effective dose according to literature is 200 mg/day.
4. Start at 0.14-0.4 mg/kg/hour if a continuous infusion is needed(6).
Oral administration of ketamine may be considered when long-term therapy is warranted for complex chronic pain patients and if other therapeutic options have failed. Generally, patients who have responded to systemic administration of ketamine are more likely to benefit from the oral form. Ketamine can be taken orally in divided doses (ranging from every 4 hours to every 12 hours). The duration of treatment depends on the intensity of side effects and may range from a few months to more than a year. Data is controversial when discussing ketamine conversion from IV to PO route of administration. Some articles recommend a conversion of 1:1 between IV and PO, whereas others suggest 3:1 between IV and PO since blood levels of the metabolite norketamine are two to three times higher with oral dosing(4,5,6).
Ketamine has both hydro- and lipophilic properties and is widely distributed throughout the body and crosses the blood-brain barrier(7). Depending on the route of administration, it has a general onset of action of 15-20 minutes.
No dose adjustments are required for renal or hepatic impairment according to the manufacturer’s labeling. Ketamine has a higher bioavailability after IM or IV administration, with an oral bioavailability of only around 20%.
The primary metabolic pathway involves hepatic N-demethylation via the cytochrome P450 system, with ketamine being a substrate for the CYP2B6, CYP2C9 and CYP3A4 cytochromes(5). Ketamine’s primary metabolite is norketamine, which is about 1/5 to 1/3 as potent as parenteral ketamine as an anesthetic agent, but equipotent when considering analgesia. An interesting fact to note is that blood concentrations of norketamine are greater (by two-three times) after oral administration compared to injectable administration(4,6). The half-life of ketamine is about two-three hours and approximately four hours for norketamine(5). It is mainly excreted renally (about 90%) with only about 5% excreted through feces.
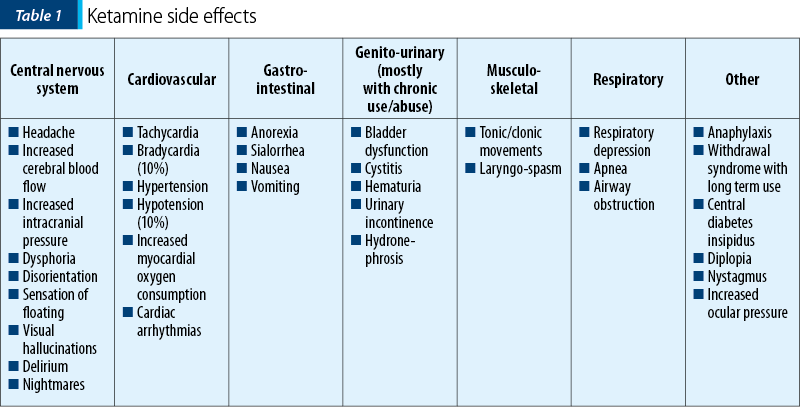
Ketamine has numerous side effects (Table 1). Psychotomimetic side effects, with a 5-35% incidence, tend to be more frequent in females, and are the main reason for the discontinuation of ketamine in pain clinics(2,4). Cardiovascular side effects may sometimes require the use of antihypertensives during infusion, along with continuous telemetry and pulse oximetry monitoring; however, these may not be required in palliative care settings. Central nervous system side effects could be minimized by pretreating patients with anxiolytics and antipsychotics, starting ketamine at low doses with slow titration, and controlling the patient’s immediate environment to decrease stimulation (dimming overhead lights, covering the patient’s eyes, using headphones and limiting the number of visitors). It was suggested that starting ketamine infusions at night may also limit side effects(2,4,6,10,13).
Contraindications to ketamine use include history of seizures, head trauma, uncontrolled intracranial hypertension due to brain metastases or hydrocephalus, schizophrenia, prior allergic reaction to ketamine, severe hypertension, congestive heart failure, recent myocardial infarction and recent MAO-I use(2,13). Caution should be used when ketamine is administered in conjunction with CYP3A4 inhibitors or CYP2C9 inducers or with medications that could enhance its CNS depressant effects such as opioids. Once again, such precautionary measures may not be warranted in the palliative care setting.
Clinicians must not omit the risk for abuse posed by ketamine when prescribing it on long term. Ketamine is structurally similar with phencyclidine (PCP) and could cause hallucinogenic and euphoric effects. Due to these effects that may last for one to two hours, ketamine gained some notoriety as a club drug. Outside the medical setting, it is known as “Special K”, “Vitamin K”, “Special LA coke”, “Super acid”, or “KitKat”. A survey conducted in the US in 2006 estimated that approximately 2.3 million teens and adults used ketamine in their lifetime. In the UK, the number of ketamine-related deaths has increased 10-fold from 1999 to 2008. In 2011, ketamine became the third most used illicit substance in China and the most prominent drug of abuse in Hong Kong, where 60.5-85.2% of substance abusers admitted to having abused ketamine. Ketamine abuse could cause damage to the cardiovascular, genitourinary, respiratory, gastrointestinal and immune systems(3,14,15). It is therefore imperative to weigh the risks and benefits in patients with a history of drug abuse or those at high risk for drug abuse.
Despite overwhelming evidence in favor of ketamine, several prestigious guiding forums recommend more research before completely embracing ketamine as an analgesic agent. While the European Society for Medical Oncology (ESMO) guidelines mention that ketamine may be helpful for patients with cancer-related neuropathic pain, the National Comprehensive Cancer Network (NCCN) states there is limited data justifying the use of ketamine for the management of cancer pain(16,17). Clinical experience, however, tells us a different story. We have successfully used ketamine in various forms for numerous patients with difficult-to-treat painful conditions.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- Namukwaya E, Leng M, Downing J, Katabira E. Cancer Pain Management in Resource-Limited Settings: A Practice Review. Pain Research and Treatment. 2011; vol. 2011, 393404, doi: 10.1155/2011/393404, PMCID: PMC3236429, PMID: 22191020.
- Allen AC, Ivester Jr. JR. Low-Dose Ketamine for Postoperative Pain Management. Journal of PeriAnesthesia Nursing. 2018 Aug; 33(4):389-398. doi: 10.1016/j.jopan.2016.12.009. Epub 2017 Jun 10.
- DeWilde KE, Levitch CF, Murrough JW, Mathew SJ, Iosifescu DV. The promise of ketamine for treatment-resistant depression: current evidence and future directions. Annals of the New York Academy of Sciences. 2015 May; 1345(1): 47-58, doi: 10.1111/nyas.12646, PMCID: PMC4447578, NIHMSID: NIHMS644818, PMID: 25649308.
- Fitzgibbon EJ, Hall P, Schroder C, Seely J, Viola R. Low dose ketamine as an analgesic adjuvant in difficult pain syndromes: a strategy for conversion from parenteral to oral ketamine. Journal of Pain and Symptom Management. 2002 Feb; 23(2):165-70, PMID: 11844639.
- Blonk MI, Koder BG, van den Bemt PMLA, Huygen FJPM. Use of oral ketamine in chronic pain management: a review. European Journal of Pain. 2010 May; 14(5):466-72, doi: 10.1016/j.ejpain.2009.09.005, Epub 2009 Oct 29.
- Graham Hocking G, Cousins MJ. Ketamine in Chronic Pain Management: An Evidence-Based Review. Anesthesia & Analgesia. 2003 Dec; 97(6):1730-9.
- Cohen SP, Bhatia A, Buvanendran B, Schwenk ES, Wasan AD, Hurley RW, Viscusi ER, Narouze S, Davis FN, Ritchie EC, Lubenow TR, Hooten WM. Consensus Guidelines on the Use of Intravenous Ketamine Infusions for Chronic Pain From the American Society of Regional Anesthesia and Pain Medicine, the American Academy of Pain Medicine, and the American Society of Anesthesiologists. Regional Anesthesia and Pain Medicine. 2018 Jul; 43(5): 521–546, doi: 10.1097/AAP.0000000000000808, PMCID: MC6023575, PMID: 29870458
- Stotz M, Oehen HP, Gerber H. Histological Findings After Long-Term Infusion of Intrathecal Ketamine for Chronic Pain: A Case Report. Journal of Pain and Symptom Management. September 1999; Vol. 18 No. 3, PMID:10517045.
- Nielsen RV, Fomsgaard JS, Siegel H, Martusevicius R, Nikolajsen L, Dahl JB, Mathiesen O. Intraoperative ketamine reduces immediate postoperative opioid consumption after spinal fusion surgery in chronic pain patients with opioid dependency: a randomized, blinded trial. PAIN. March 2017, Volume 158 (3), p 463-470, doi: 10.1097/j.pain.0000000000000782, ISSN: 0304-3959
- Allen CA, Ivester Jr JR. Ketamine for Pain Management-Side Effects & Potential Adverse Events. Pain Management Nursing. 2017 Dec; 18(6):372-377. doi: 10.1016/j.pmn.2017.05.006, PMID: 28743507.
- Boenigk K, Echevarria GC, Nisimov E, von Bergen Granell AE, Cuff GE, Wang J, Atchabahian A. Low-dose ketamine infusion reduces postoperative hydromorphone requirements in opioid-tolerant patients following spinal fusion: A randomised controlled trial. European Journal of Anesthesiology. 2018 Aug 14, doi: 10.1097/EJA.0000000000000877
- Fine PG. Low-dose ketamine in the management of opioid nonresponsive terminal cancer pain. Journal of Pain and Symptom Management. April 1999; Vol. 17 No. 4, PMID: 10203883.
- Clifford T. Ketamine for pain management. Journal of PeriAnesthesia Nursing. 2012 Dec; 27(6):423-4. doi: 10.1016/j.jopan.2012.09.004., PMID: 23164210
- Liu Y, Lin D, Wu B, Zhou W. Ketamine abuse potential and use disorder. Brain Research Bulletin. September 2016; Vol. 126, Part 1, Pages 68-73, doi.org/10.1016/j.brainresbull.2016.05.016.
- Lee EE, Della Selva MP, Liu A, Himelhoch S. Ketamine as a novel treatment for major depressive disorder and bipolar depression: a systematic review and quantitative meta-analysis. General Hospital Psychiatry. 2015 Mar-Apr; 37(2):178-84. doi: 10.1016/j.genhosppsych.2015.01.003, PMID: 25698228.
- Fallon M, Giusti R, Aielli F, Hoskin P, Rolke R, Sharma M, Ripamonti CI. ESMO Guidelines Committee; Management of cancer pain in adult patients: ESMO Clinical Practice Guidelines. Annals of Oncology. 1 October 2018; Volume 29, Issue Supplement 4, Pages iv166–iv191, https://doi.org/10.1093/annonc/mdy152
- NCCN Guidelines for Adult Cancer Pain, version 1.2018.NCCN.org