The process of invagination of a proximal section of the intestine (intussusceptum) into the neighbouring distal part (intussuscipiens) is known as intussusception. We hereby present the case report of a 39 years-old man presenting to the emergency room with colicky abdominal pain increasing in intensity in the past few months. The imagery indicated a small bowel tumour triggering intussusception, but falsely assumed it was a GIST. The surgical intervention, mainly dictated by the acute setting of small bowel obstruction found a small bowel tumour causing intussusception – enterectomy of the affected intestinal segment was performed with stapled anastomosis. The postoperative course was favourable and uneventful, the pathology exam revealed the nature of the tumour: a small bowel metastasis from an achromic melanoma, of unknown origin. The patient is currently on a specific treatment for metastatic malignant melanoma (BRAF inhibitor and MEK inhibitor), with a good clinical outcome at 5 months after surgery (disappearance of the abdominal pain, of the anorexia and weight gain).
O metastază a intestinului subţire dintr-un melanom acromic, provocând invaginaţie şi ocluzie intestinală – prezentare de caz
A small bowel metastasis from an achromic melanoma causing intussusception and bowel obstruction – a case presentation
First published: 20 decembrie 2021
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/OnHe.57.4.2021.5799
Abstract
Rezumat
Procesul de telescopare a unei secţiuni proximale intestinale (intussusceptum) în partea distală vecină (intussuscipiens) este cunoscut sub numele de invaginaţie intestinală. Prezentăm cazul unui bărbat în vârstă de 39 de ani care s-a prezentat în urgenţă, având colici abdominale care au crescut în intensitate în ultimele luni. Imagistica efectuată a indicat prezenţa unei formaţiuni tumorale a intestinului subţire care cauzase invaginaţia respectivă, suspectându-se în mod eronat un GIST. Intervenţia chirurgicală, dictată în principal de contextul clinic acut (ocluzie intestinală), a constatat o tumoră a intestinului subţire cu invaginaţie. S-a practicat enterectomia segmentului intestinal afectat, cu anastomoză mecanică. Evoluţia postoperatorie a fost favorabilă şi fără incidente, iar examenul patologic a identificat natura tumorii: o metastază la nivelul intestinului subţire, provenind de la un melanom acromic, cu punct de plecare necunoscut. Pacientul se află în prezent sub tratament specific pentru melanom malign metastatic (inhibitor BRAF şi inhibitor MEK), cu un rezultat clinic bun la 5 luni după intervenţia chirurgicală (dispariţia durerilor abdominale, a anorexiei şi creştere în greutate).
Background
The invagination of a proximal section of the intestine into the neighboring distal part is known as intussusception. This article describes the diagnostic challenge and treatment management of a 39-year-old man with a rare condition: a stage IV achromic malignant melanoma causing intussusception and small bowel obstruction.
While intussusception is common in children, typically manifesting as cramping abdominal pain, bloody diarrhea and a palpable painful mass, it is uncommon in adults.
Considered a rare condition, it accounts for 5% of all intussusceptions and nearly 1-5% of bowel obstruction, according to a research performed by Marinis et al.(1)
Adult intussusception differs from pediatric intussusception in a number of aspects, including the genesis, clinical features, and treatment options. In contrast to intussusceptions in children, in the adult the process has an organic cause in the majority of instances. Examples of etiologic agents are: inflammatory bowel disease, postoperative adhesions, Meckel’s diverticulum, benign and malignant lesions, metastatic neoplasms or even iatrogenic, due to the presence of intestinal tubes, jejunostomy feeding tubes or after gastric surgery.
The surgical intervention is frequently recommended in the adult(2). In a study performed by Hong et al.(3), it was found that the most common cause of malignant tumor in intestinal intussusception was metastatic cancer. Primary adenocarcinoma, on the other hand, was the most common source of malignant tumor in ileocolic and colonic intussusception.
According to a research performed by Silva et al.(4), the gastrointestinal tract is frequently affected by metastatic malignant melanoma (60%). Because most patients are asymptomatic, only 1-4% of melanoma metastases to the gastrointestinal tract are discovered before death.
In individuals with digestive complaints or ferropenic anemia, gastrointestinal spread of a previously treated malignant melanoma should always be considered. Intestinal melanoma metastases can appear with symptoms such as small bowel intussusception and gastrointestinal bleeding.
The surgical excision remains the gold standard of treatment, not just for symptom relief, but also for enhanced survival.
Case presentation and clinical setting
Frequently, in the case of intussusception, the patient will present with nonspecific concerns that have been bothering him for a long time. Because of the nonspecific indications and symptoms, diagnosing intussusception in adults can be difficult(5).
As shown in research performed by Shenoy and Cassim(6), and mentioned previously, malignant melanoma is a rare metastatic tumor that affects the gastrointestinal tract, with the small bowel being the most common site of involvement. Acute abdominal emergencies – such as intestinal obstruction, intussusception, hemorrhage and perforation – can show up in a clinical context, along with persistent (or chronic) symptoms, such as weight loss, abdominal pain and anemia.
We present the case of a 39-year-old man who addressed the emergency room for intense diffuse abdominal pain which did not respond to painkillers self-administered orally. The pattern of the pain was: colicky, with a maximum felt in the left flank, a pain that had been evolving and increasing in intensity in the previous four months, and which associated anorexia, weight loss and fatigability.
Investigations and diagnosis
In children, the diagnosis is commonly suspected before performing the imaging, but in adults it is frequently made unexpectedly. Plain film radiography, barium tests and ultrasound imaging, all play important roles in the diagnosis and therapy of this condition, and CT and MRI scans are becoming more popular, especially in the adult population(7).
Due to the fact that an edematous or hemorrhagic intussuscipiens might mimic a tumor on each modality, determining the existence of a malignant lead point remains difficult. Although bowel viability markers have been described, they are not accurate(8).
According to research conducted by Marinis et al.(1), the most sensitive diagnostic modality is computed tomography, which can distinguish between different types of intussusceptions, with and without a lead point. Differentiating between lead point and non-lead point intussusception is critical for selecting the best treatment and may avoid the need for unnecessary surgery(9). Computed tomography findings are pathognomonic for this condition(10).
Colonoscopy can detect most lead point lesions of non-enteric intussusceptions(11). In most cases, radiologists can easily diagnose intestinal intussusception by observing the characteristic bowel-within-bowel look on an abdominal CT scan.
In a study(12) targeting the comparison between phase-inversion harmonic imaging (PIHI) and standard B-mode ultrasonography (US) in the examination of bowel pathology, PIHI improved bowel sonography by increasing overall image quality and allowing for improved visualization of bowel pathology and accompanying alterations, with a benefit of providing approximately 20% more accurate information.
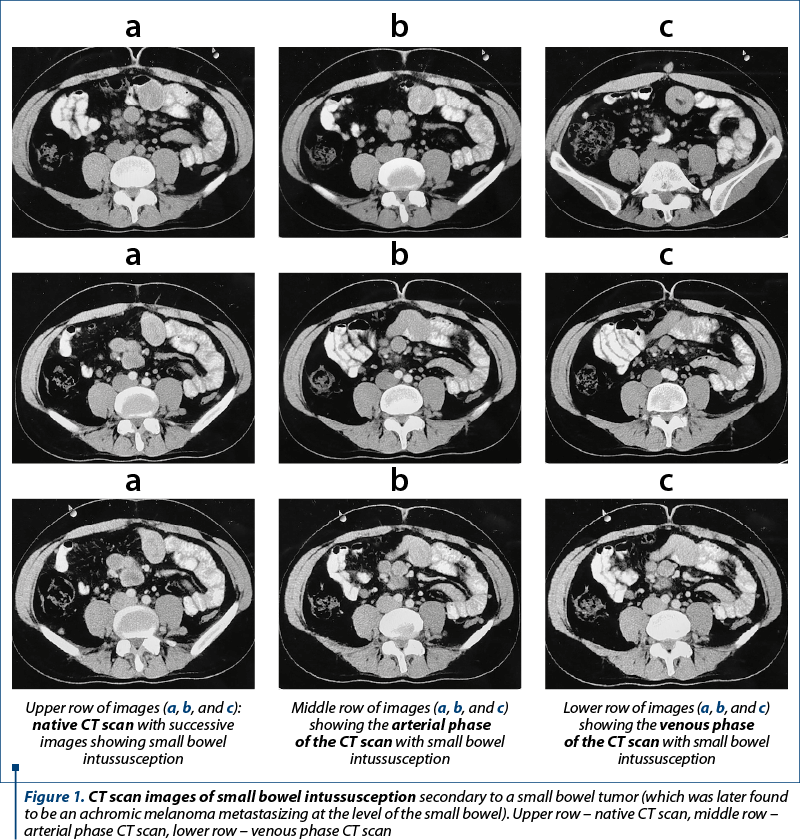
The subject of our case presentation addressed the emergency department with a CT scan which described “a small bowel loop at the level of the mesogastrium, discretely invaginated through the presence of a voluminous tumor, also associating multiple peritoneal nodules, bilateral lung nodules, and a left lobulated diaphragmatic mass. The conclusion of the present CT scan exam is: small bowel mass with an aspect suggestive for a GIST tumor, with secondary determinations to the lungs, a right axillary increased lymph node, peritoneal carcinomatosis.” The above description from the report of the CT scan, confusing a metastatic melanoma and taking it for a GIST, was a phenomenon underlined by Ye et al.(13) and Gabali et al.(14) in studies that showed similarities between the two conditions.
Surgical treatment
In the conclusion stated in the study conducted by Marinis et al.(1), adult intussusceptions can only be treated with surgery. On the other hand, in a research done by Eisen et al.(15), the data presented supported a selective approach to the operative treatment of intussusception in adults.
Every case in which a cancer is detected is treated with a formal bowel resection based on oncological principles. In certain instances, reducing the intussuscepted bowel is regarded safe for benign lesions in order to restrict the extent of resection or to avoid small bowel syndrome. In a paper presented by Silva et al.(4), small bowel intussusception was linked to malignancy in 31% of cases (43/137) and large bowel intussusception in 70% of cases (74/106).
The theoretical background for the surgical approach can rely on research performed by Fiordaliso et al.(2), which mentions that enteric intussusception can be treated with reduction and resection and that, on the contrary, colonic intussusception should be removed in its entirety. The literature discusses the possibility of not operating on adult intussusception, but this option is pertinent in cases where the intussusception is intermittent, as shown by Aydin et al.(16) Adult intussusception is still treated with surgery, mainly because most of the patients have intraluminal lesions and there is consistent possibility that those lesions are malignant. As mentioned before, we further enhance the idea that surgery was firmly indicated in this case: 1) as a means to solve the bowel obstruction and the abdominal pain syndrome, with the latter persisting for months; 2) in order to have a complete and reliable diagnosis, and 3) the tumor was bleeding, causing secondary anemia.
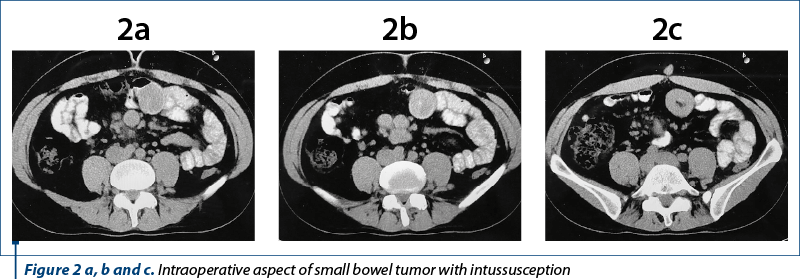
In the case of our patient, we intervened surgically and we entered the peritoneal cavity where we found an area of invagination (during the inspection of the bowel loops), we reduced the process and found within a small bowel tumor, a level at which we performed an enterectomy with a further stapled anastomosis and we also biopsied two peritoneal nodules and one intraaponeurotic nodule which was obviated at the moment of closure of the abdomen. All the specimens were sent to the pathology department in order to establish the etiology of the disease.
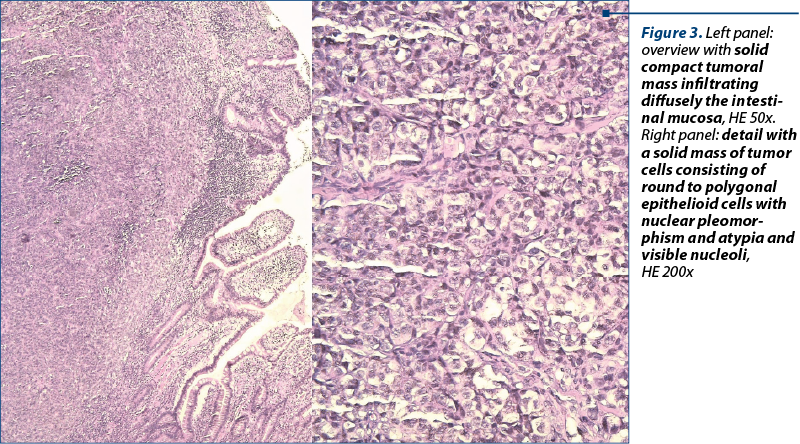
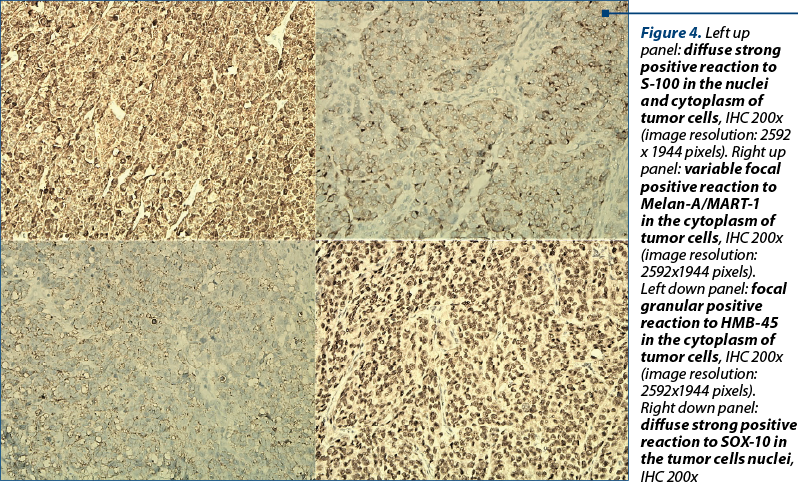
Pathology result
The final pathology result was small bowel metastasis from an achromic melanoma. In his previous medical history, the patient had a tumor resection from a plantar melanoma, without being able to provide more specific details, and the previous pathology report was not available. A dermatology consultation was asked and the identification of the primary (achromic) malignant melanoma was not possible.
Treatment completion after the pathology result
The treatment indicated by the oncologist after the complete and correct diagnosis established in the pathology department was with dabrafenib and trametinib.
Conclusions
The gastrointestinal tract is frequently affected by malignant melanoma. The disease is mostly asymptomatic, being frequently diagnosed only after complications arise. Intussusception of the small bowel and gastrointestinal hemorrhage are uncommon manifestations of metastatic melanoma, with only a few cases described, as shown by Silva et al.(4)
Any patient with a history of cutaneous melanoma and new gastrointestinal symptoms should be suspected of having metastatic gastrointestinal melanoma, a situation also described in a study performed by Shenoy and Cassim(6). The surgical procedures for symptomatic patients with gastrointestinal melanoma reduce the discomfort and enhance the quality of life, and they may even increase survival.
Outcome, prognosis and follow-up
At the population level, survival following diagnosis of amelanotic melanoma is lower than that following diagnosis of pigmented melanoma, as demonstrated in a study conducted by Thomas et al.(17) Because amelanotic melanomas are difficult to diagnose, they are likely to present at more advanced tumor stages.
The presence of mitoses in amelanotic melanoma, regardless of Breslow thickness or other clinicopathologic characteristics, suggests that amelanotic melanomas may also grow more rapidly than pigmented melanomas. At the moment of the completion of this article, the patient is alive and in a good clinical condition (the abdominal pain and the anorexia disappeared, and the patients gained weight) five months after surgery. We emphasize the fact that, from the moment the patient addressed our clinic, and judging by the result of his CT scan, the diagnosis was stage 4 of disease, and the main purpose of the surgery was to solve the emergency setting and, of course, to indicate the proper diagnosis. The improvement in the patient’s general condition is, nevertheless, due to the proper oncologic treatment, administered after the resolution of the acute condition (the intussusception with bowel obstruction). The multidisciplinary collaboration is critical to provide the best care possible for our patients.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
-
Marinis A, Yiallourou A, Samanides L, Dafnios N, Anastasopoulos G, Vassiliou I, Theodosopoulos T. Intussusception of the bowel in adults: a review. World J Gastroenterol. 2009 Jan 28;15(4):407-11. doi: 10.3748/wjg.15.407.
-
Fiordaliso M, Panaccio P, Costantini R, De Marco AF. Comparison between children and adults intussusception. Description of two cases and review of literature. Ann Ital Chir. 2021;92:268-276.
-
Hong KD, Kim J, Ji W, Wexner SD. Adult intussusception: a systematic review and meta-analysis. Tech Coloproctol. 2019 Apr;23(4):315-324. doi: 10.1007/s10151-019-01980-5.
-
Silva S, Tenreiro N, Melo A, Lage J, Moreira H, Próspero F, Avelar P. Metastatic melanoma: An unusual cause of gastrointestinal bleeding and intussusception – A case report. Int J Surg Case Rep. 2018;53:144-146. doi: 10.1016/j.ijscr.2018.10.057.
-
Aref H, Nawawi A, Altaf A, Aljiffry M. Transient small bowel intussusception in an adult: case report with intraoperative video and literature review. BMC Surg. 2015 Apr 3;15:36. doi: 10.1186/s12893-015-0020-6.
-
Shenoy S, Cassim R. Metastatic melanoma to the gastrointestinal tract: role of surgery as palliative treatment. W V Med J. 2013 Jan-Feb;109(1):30-3. https://pubmed.ncbi.nlm.nih.gov/23413546/
-
Byrne AT, Geoghegan T, Govender P, Lyburn ID, Colhoun E, Torreggiani WC. The imaging of intussusception. Clin Radiol. 2005 Jan;60(1):39-46. doi: 10.1016/j.crad.2004.07.007. Erratum in: Clin Radiol. 2005 Mar;60(3):412.
-
Huang BY, Warshauer DM. Adult intussusception: diagnosis and clinical relevance. Radiol Clin North Am. 2003 Nov;41(6):1137-51. doi: 10.1016/s0033-8389(03)00116-7.
-
Kim YH, Blake MA, Harisinghani MG, Archer-Arroyo K, Hahn PF, Pitman MB, Mueller PR. Adult intestinal intussusception: CT appearances and identification of a causative lead point. Radiographics. 2006 May-Jun;26(3):733-44. doi: 10.1148/rg.263055100.
-
McKay R. Ileocecal intussusception in an adult: the laparoscopic approach. JSLS. 2006 Apr-Jun;10(2):250-3: https://pubmed.ncbi.nlm.nih.gov/16882431/
-
Wang N, Cui XY, Liu Y, Long J, Xu YH, Guo RX, Guo KJ. Adult intussusception: a retrospective review of 41 cases. World J Gastroenterol. 2009 Jul 14;15(26):3303-8. doi: 10.3748/wjg.15.3303.
-
Schmidt T, Hohl C, Haage P, Honnef D, Mahnken AH, Krombach G, Piroth W, Günther RW. Phase-inversion tissue harmonic imaging compared to fundamental B-mode ultrasound in the evaluation of the pathology of large and small bowel. Eur Radiol. 2005 Sep;15(9):2021-30. doi: 10.1007/s00330-005-2749-2.
-
Ye Z, Yang Z, Zheng S, Wang W. Robot-assisted laparoscopic surgery for abdominal metastatic melanoma mimicking a gastrointestinal stromal tumor: A case report and review of the literature. Medicine (Baltimore). 2018 Jun;97(26):e11207, doi: 10.1097/MD.0000000000011207.
-
Gabali AM, Priebe P, Ganesan S. Primary melanoma of small intestine masquerading as gastrointestinal stromal tumor: a case report and literature review. Am Surg. 2008 Apr;74(4):318-21. PMID: 18453296
-
Eisen LK, Cunningham JD, Aufses AH Jr. Intussusception in adults: institutional review. J Am Coll Surg. 1999 Apr;188(4):390-5. doi: 10.1016/s1072-7515(98)00331-7.
-
Aydin N, Roth A, Misra S. Surgical versus conservative management of adult intussusception: Case series and review. Int J Surg Case Rep. 2016;20:142-6. doi: 10.1016/j.ijscr.2016.01.019.
-
Thomas NE, Kricker A, Waxweiler WT, et al. Comparison of clinicopathologic features and survival of histopathologically amelanotic and pigmented melanomas: a population-based study. JAMA Dermatology. 2014 Dec;150(12):1306–1314. doi: 10.1001/jamadermatol.2014.1348.
Articole din ediţiile anterioare
Malignant melanoma of the leg – challenges. A case report
Melanomul malign cutanat este al 15-lea cancer ca frecvenţă în rândul femeilor, iar incidenţa şi mortalitatea asociate melanomului malign continuă ...