The importance of detailed knowledge of the morphology and morphometry of the inferior orbital fissure and its anatomical variations is particularly important for surgeons who approach this area in order to avoid injuries of the neurovascular bundles that pass through. We performed a study in which we evaluated the morphology and morphometry of the inferior orbital fissure using laser technology so that the topography and measurements be as accurate as possible. The study was performed by scanning 30 dry adult human skulls (60 orbits) in order to identify the anatomical variants and to measure the diameters of the inferior orbital fissure. Analyzing the data, we noticed that the average length of the inferior orbital fissure is 33.5 mm, and the average width is 5.01 mm. A thorough knowledge of the anatomical variants of the inferior orbital fissure and its dimensions may be useful to surgeons who address this complex anatomical area in order to avoid the important anatomical structures that pass through this fissure.
Variaţiile morfologice şi morfometrice ale fisurii orbitare inferioare
Morphological and morphometric variation of the inferior orbital fissure
First published: 09 aprilie 2021
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/ORL.51.2.2021.5430
Abstract
Rezumat
Importanţa cunoaşterii detaliate a morfologiei şi morfometriei fisurii orbitare inferioare şi a variaţiilor sale anatomice este indispensabilă pentru chirurgii care abordează această zonă, cu scopul de a evita leziunile structurilor vasculo-nervoase care străbat această regiune. Am efectuat un studiu în care am evaluat morfologia şi morfometria fisurii orbitare inferioare folosind tehnologia laser, astfel încât topografia şi măsurătorile să fie cât mai precise. Studiul a fost realizat prin scanarea a 30 de cranii umane adulte (60 de orbite), cu scopul de a identifica variantele anatomice şi de a măsura diametrele fisurii orbitare inferioare. Analizând datele, am observat că lungimea medie a fisurii orbitare inferioare este de 33,5 mm şi lăţimea medie este de 5,01 mm. O cunoaştere aprofundată a variantelor anatomice ale fisurii orbitare inferioare şi a dimensiunilor acesteia poate fi utilă medicilor care intervin chirurgical asupra acestei zone anatomice complexe, pentru a evita lezarea structurilor anatomice importante care au sediul în această regiune a orbitei.
Introduction
The inferior orbital fissure (IOF) – or sphenomaxillary fissure – is a bony cleft that separates the lateral and the inferior orbital wall in their posterior part. In the superolateral part, it is limited by the great wing of the sphenoid and by the zygomatic bone and in the inferomedial part it is limited by the orbital process of the palatine bone and the maxillary bone(1,2). A number of vasculonervous structures cross this fissure: the terminal branches of the maxillary artery and related veins, the infraorbital and zygomatic branches of the maxillary nerve (V2), the orbital postganglionic parasympathetic branches of the pterygopalatine ganglion and the inferior ophthalmic vein(2). IOF separates the orbit from the infratemporal fossa and the pterygopalatine fossa(1), thus allowing infectious, tumor or traumatic lesions to lie between these anatomical regions(3).
The inferior orbital fissure may have different anatomical variations and a detailed knowledge of the variations is important in avoiding vascular or nerve damage. The inferior orbital fissure is an important landmark during surgical access to the posterior orbital floor(4), optic nerve decompression(5), orbital decompression(5,6), maxillofacial surgery(7) or cranial base surgery(8).
We did not find in the specialized literature morphometric or morphological data obtained with laser technology on population groups from Romania or from other populations. These measurements can be of great importance for surgeons who approach this area, in preoperative planning and in avoiding intraoperative complications. Also, these data can be useful to manufacturers of orbital wall prostheses for the realization of prostheses with the most exact dimensions that correspond to the local orbital morphometry.
Materials and method
The study was conducted within the Anatomy Discipline of the “Carol Davila” University of Medicine and Pharmacy Bucharest and within the “Fr. I. Rainer” Institute of Anthropology of the Romanian Academy. Our study was performed on 30 dry skulls (60 orbits) that were included in the study and were scaned with laser and then analyzed. For each analyzed skull, the sex and the location of the orbit (right/left) were noted. The distribution by sex in the studied group was equal, 15 skulls belonged to men and 15 to women.
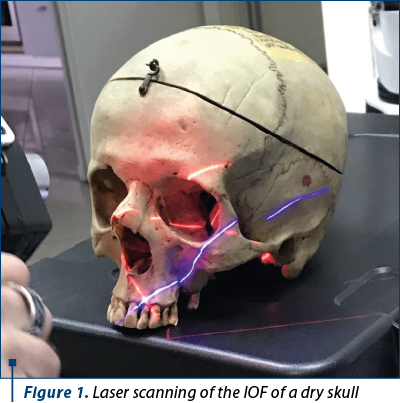
Dry skull laser scans were performed within the Hexagon Manufacturing Intelligence Company, Bucharest. This company is one of the most reputable names in measurement and metrology for more than 200 years. We scaned the orbits with RS6 laser scanner that was placed on an arm with multiple articulated joints that facilitates handling of the scanner and maximize accuracy (Figure 1).
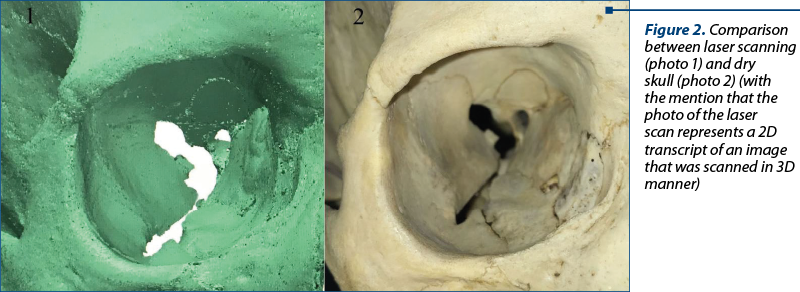
The RS6 laser scanner has an accuracy of 0.026 mm, it can scan up to 1.2 million points/second and the minimum distance between scanned points is 0.027 mm. For each orbit, the laser scanned approximately 20 million points. The RS6 laser scanner was connected to a software, Polyworks Inspector Premium program (developed by InnovMetric, Quebec, Canada), that allowed the real-time visualization of scans that we performed. This program has a three-dimensional analysis software solution with the help of which we performed the measurements at the level of the inferior orbital fissure (Figure 2).
For each orbit, the IOF morphology was observed and it was divided into several types.
The parameters that were measured bilaterally included:
-
the entire length of the IOF
-
the width of the IOF, which was measured in every third of the IOF.
The data that were obtained were analyzed statistically using MS Office, 2010 Excel spread sheet (Microsoft Corp., Redmond, WA).
Results and discussion
We analyzed the images of the laser scans and we observed six types of IOF (Figure 3):
Type 1 – IOF has a narrow posteromedial part and a wider anterolateral part.
Type 2 – IOF is very narrow along its entire length.
Type 3 – IOF has a rectangular shape.
Type 4 – IOF resembles the letter “V”, with a longer posterior segment and shorter anterior segment.
Type 5 – IOF has a very narrow posteromedial segment and a wider anterolateral part.
Type 6 – IOF presented a wider area at each end of the fissure and a narrower segment in the middle.
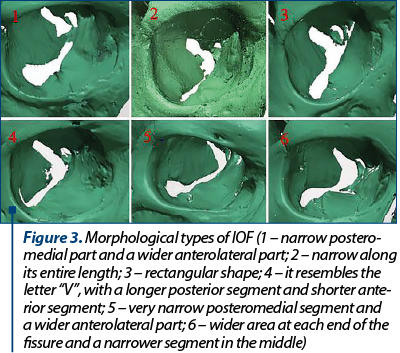
Our results are largely similar to the types of IOF that Ozer et al.(9) described in their study, with the mention that in their study they described eight morphological types of IOF. The morphological types that we did not find in the skulls we analyzed were represented by the IOF that had a triangular shape and those that had a tear drop appearance.
Studying the 30 skulls, we noticed that the morphology of the IOF tends to be right/left symmetrical (27 skulls), and only in the case of three skulls we noticed a discrepancy between the morphologies of the IOF: in the first skull the right orbit had an IOF type 3 and in the left orbit an IOF type 5; in the case of the second skull, the IOF from the right orbit was type 2 and the one from the left orbit was type 5, and in the case of the third skull, the right IOF was type 5 and the left one was type 6.
Regarding the frequency of each type, by far, type 1 was the most common morphology of IOF that we found, followed by type 5, with a lower frequency but in similar proportions there were types 2 and 3, and the rarest morphologies were represented by types 4 and 6. Of the 60 orbits we analyzed, type 1 represented 40%, types 2 and 3 each represented 11.66%, type 4 totaled 6.66%, type 5 represented 23.33% and type 6, similar to type 4, totaled 6.66%.
The average length of the IOF was 33.5 mm. The average length of the IOF in the right orbit was 33.4 mm and in the left one, 33.6 mm. The right IOF in men was 33.45 mm (variation between 32.9 and 40.2 mm), while in women it was 32.35 mm (variation between 29.86 and 37.34 mm). The left IOF in men had an average of 33.19 mm (variation between 27.3 and 38.38 mm) and in women it was 34.01 mm (variation between 28.77 and 38.51 mm). The mean length of IOF in men was 33.82 mm and in women it was 33.18 mm. From these data, we can observe that the length of the IOF is slightly longer in men compared to women, and that the left IOF was usually slightly longer than the right.
The average width of the IOF in men was 4.73 mm, while in women it was 5.3 mm. The average width of the IOF in the right orbit was 4.94 mm and in the left orbit it was 5.09 mm. The average width of the IOF in its anterior third was 6.32 mm, in the middle third it was 4.24 mm, and in the posterior third it was 4.41 mm. Looking at these values, we can observe that women generally have a wider IOF than men. The IOF in the left orbit is not only slightly longer, but is also slightly wider than in the right orbit. Analyzing the average widths of the IOF in each measured third, we can see that the largest width is found in the anterior third, then the fissure becomes narrower in the middle third and then becomes slightly wider in the posterior third. Comparing these mesurements with the data obtained from literature, we notice that both the length and the widths of the IOF are larger than those obtained by De Bastista et al. in their study(8).
These landmarks are important for locating and identifying IOF morphology and size, especially during surgeries involving the lateral wall of the orbit which can lead to important complications, such as diplopia, enophthalmia, orbital hemorrhage or ocular dysfunction(10).
Conclusions
The inferior orbital fissure tends to be symmetrical in morphology in the two orbits.
The length of the IOF is slightly longer in men compared to women, and the left IOF was usually slightly longer than the right one.
The width of the IOF tends to follow a pattern, being wider in the anterior third, narrow to the middle third, and in the posterior third being slightly wider than in the middle third.
Knowing the variability of the morfology and morphometry of the IOF by surgeons who approach this anatomic area is important for protecting the vasculonervous bundles that pass through the fissure. This will prevent injury of the vessels and nerves during orbital decompression or in the interventions at the base of the skull with access from this area.
Bibliografie
-
Engin Ö, Adriaensen GFJPM, Hoefnagels FWA, Saeed P. A systematic review of the surgical anatomy of the orbital apex. Surg Radiol Anat. 2021;43(2):169-178.
-
Herzallah IR, Elsheikh EM, Casiano RR. Endoscopic endonasal study of the maxillary nerve: a new orientation. Am J Rhinol. 2007;21(5):637-43.
-
Tashi S, Purohit BS, Becker M, Mundada P. The pterygopalatine fossa: imaging anatomy, communications, and pathology revisited. Insights Imaging. 2016;7(4):589-599.
-
Ricketts S, Chew HF, Sunderland IR, Kiss A, Fialkov JA. Transection of inferior orbital fissure contents for improved access and visibility in orbital surgery.
-
J Craniofac Surg. 2014;25(2):557-562.
-
Ben Simon GJ, Syed HM, Lee S, Wang DY, Schwarcz RM, McCann JD, Goldberg RA. Strabismus after deep lateral wall orbital decompression in thyroid-related orbitopathy patients using automated hess screen. Ophthalmology. 2006;113(6):1050-5.
-
Goldberg RA, Kim AJ, Kerivan KM. The lacrimal keyhole, orbital door jamb, and basin of the inferior orbital fissure. Three areas of deep bone in the lateral orbit. Arch Ophthalmol. 1998;116(12):1618-24.
-
Aldridge T, Thomson A, Ilankovan V. Abnormal anatomy of inferior orbital fissure and herniation of buccal fat pad. Br J Oral Maxillofac Surg. 2015;53(1):92-93.
-
De Battista JC, Zimmer LA, Theodosopoulos PV, Froelich SC, Keller JT. Anatomy of the inferior orbital fissure: implications for endoscopic cranial base surgery.
-
J Neurol Surg B Skull Base. 2012;73(2):132-138.
-
Ozer MA, Celik S, Govsa F. A morphometric study of the inferior orbital fissure using three-dimensional anatomical landmarks: application to orbital surgery. Clin Anat. 2009;22(6):649-654.
-
Unal M, Leri F, Konuk O, Hasanreisoğlu B. Balanced orbital decompression combined with fat removal in Graves ophthalmopathy: do we really need to remove the third wall?. Ophthalmic Plast Reconstr Surg. 2003;19(2):112-118.