Adolescent pregnancy represents a major health problem worldwide, because it is associated with multiple maternal and fetal complications, the most important one being maternal death. According to the specialty literature, the leading cause of death among adolescents is represented by adverse outcomes associated with pregnancy. Also, in this group of patients there is a high risk of sexually transmitted diseases. The most common obstetrical complications in pregnant adolescents are preeclampsia and eclampsia, which increase the risk of maternal and fetal mortality. Regarding the neonatal outcomes, it has been demonstrated that newborns from adolescent patients have a higher risk of preterm birth, low birth weight and stillbirth. All these complications may be due to the physical and biological immaturity, but also may be the result of the lack of antenatal care. We performed a retrospective study in the Department of Obstetrics and Gynecology of the University Emergency Hospital Bucharest between 30 September 2020 and 30 September 2022. The study included three adolescents who gave birth and were declared dead in our unit, and a control group of five adult patients with the same characteristics. The aim of the study was to establish the incidence and the risk factors of mortality among adolescents compared to adult women. The neonatal status was established by neonatology team. The results showed that the incidence of maternal mortality is higher in adolescent patients compared to the adult ones as reported to all patients who gave birth. The patients aged between 35 and 40 years old had the highest rate of mortality, followed by the group of patients aged between 18 and 19 years. The lack of antenatal care had an important significance in both groups. Fetal mortality was similar in both adolescent and adult groups.
Mortalitatea maternă şi fetală în rândul pacientelor adolescente
Maternal and fetal mortality in adolescent patients
First published: 30 noiembrie 2022
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.38.4.2022.7387
Abstract
Rezumat
Sarcina în rândul adolescentelor reprezintă o problemă majoră de sănătate publică în lumea întreagă, deoarece asociază numeroase complicaţii materno-fetale, cea mai importantă fiind reprezentată de decesul matern. Potrivit literaturii de specialitate, principala cauză de deces în rândul adolescentelor este asociată complicaţiilor sarcinii. De asemenea, în acest grup populaţional există un risc crescut de boli cu transmitere sexuală. Cele mai frecvente complicaţii obstetricale întâlnite în rândul adolescentelor gravide sunt preeclampsia şi eclampsia, care cresc semnificativ mortalitatea maternă şi fetală. În ceea ce priveşte prognosticul neonatal, s-a demonstrat că nou-născuţii proveniţi din mame adolescente au un risc crescut de naştere prematură, greutate scăzută la naştere şi de moarte fetală peripartum. Toate aceste complicaţii pot fi datorate imaturităţii fizice şi biologice, dar pot fi şi rezultatul lipsei dispensarizării adecvate a sarcinii. Am efectuat un studiu retrospectiv în Clinica de obstetrică şi ginecologie a Spitalului Universitar de Urgenţă Bucureşti, în perioada 30.09.2020-30.09.2022, care a inclus trei paciente adolescente care au născut şi au fost declarate decedate în clinica noastră şi un grup de control alcătuit din cinci paciente adulte prezentând aceleaşi caracteristici. Scopul studiului a fost de a stabili incidenţa şi factorii de risc asociaţi decesului matern în rândul pacientelor adolescente comparativ cu cele adulte. Statusul neonatal a fost evaluat de către echipa de neonatalogie. Rezultatele au evidenţiat că mortalitatea maternă este mai crescută în rândul adolescentelor comparativ cu cele adulte, raportat la numărul total de naşteri din cadrul clinicii. Cea mai ridicată incidenţă a mortalităţii a fost înregistrată în categoria de vârstă 35-40 de ani, urmată de cea cuprinsă între 18 şi 19 ani. Lipsa controalelor prenatale a avut o importanţă semnificativă în ambele grupe. Mortalitatea fetală a fost similară în cele două categorii de paciente.
Introduction
Adolescence is defined by World Health Organization (WHO) as the period of transition from childhood to adult lifetime in the population aged between 10 and 19 years old(1,2). The incidence of births among adolescents is estimated to be 12 million in girls aged between 15 and 19 years old, and 777,000 in girls below 15 years old. These numbers are related to low- and middle-income countries, which represent the majority of the cases(3-5).
The sexual behavior during adolescence presents a high risk of sexually transmitted diseases (STDs) and of unintended pregnancy(1,6). The most discussed STD is the human immunodeficiency virus (HIV) infection, because it may have consequences in every moment of life, including pregnancy. In 2016, it was estimated that more than 2 million of adolescents were HIV-positive(7-9). Despite this infection, other STDs were demonstrated to have the second incidence rate in the population group aged between 15 and 19 years old(7,10). Even though there are treatments for STDs, including HIV, the lack of medical care associates a high risk of morbidity, mortality and other complications(7,11).
Regarding the pregnancy during adolescence, studies have shown that its complications and the adverse outcomes associated to childbirth represent the main cause of death in this population, especially in developing countries(12,13). The most common complications related to adolescent pregnancy are preeclampsia and eclampsia which may have a negative impact on the maternal and fetal status, by increasing the risk of mortality(12,14). Adolescents have a double risk of death during childbirth compared to adult women(15). An important mention is that 13% of all maternal deaths worldwide occur in pregnant adolescents(15).
An analysis of data from 38 countries estimated that the risk of death per birth in girls aged between 15 and 19 years old is 28% higher than in patients aged between 20 and 24 years old(16,17). The studies are uniform; data from Australia showed that the maternal mortality is higher in adolescents compared to adult women(16,18). Research demonstrates that age is an independent risk factor for maternal mortality, therefore the risk increases as the age is lower, especially below 15 years old, even in developing and developed countries(16,19).
Also, the perinatal mortality is higher in adolescents. Studies have shown that this population has a mortality rate among infants 60% higher than those of adult patients(15,20). Stillbirth among adolescents was found to have an increased prevalence, which may be explained by various conditions such as obstetrical complications, infections during pregnancy or congenital malformations(21,22). Despite these causes, it was demonstrated that most of these outcomes are due to improper antenatal care(15).
The aim of this study is to analyze the incidence and the risk factors for maternal and fetal death among adolescent patients compared to adult ones.
Materials and method
We performed a retrospective study in the Department of Obstetrics and Gynecology of the University Emergency Hospital Bucharest during a period of two years, between 30 September 2020 and 30 September 2022. We analyzed adolescent patients who delivered and were declared dead after birth in our hospital. The neonatal status was assessed by birth weight and by the 1-minute Apgar score given by neonatology team. The study included three adolescent patients who were declared dead during the two analyzed years, and a control group of five adult patients with the same characteristics.
The information regarding pregnancy and neonatal data was retrieved from the hospitalization sheets and the Base Data System of the University Emergency Hospital Bucharest. Maternal age was defined as that recorded at the time of hospital admission.
Results
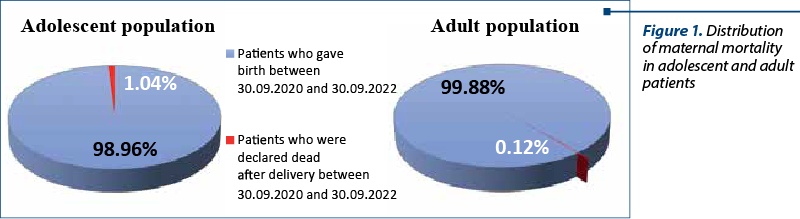
In the analyzed period of time, there were eight patients declared dead after delivery, representing a percentage of 0.19% of all patients who delivered in our unit. Regarding the stratification cases in adolescent and adult patients, the rate of maternal mortality among adolescents was 1.04%, while in adult group it was 0.12% (Figure 1).
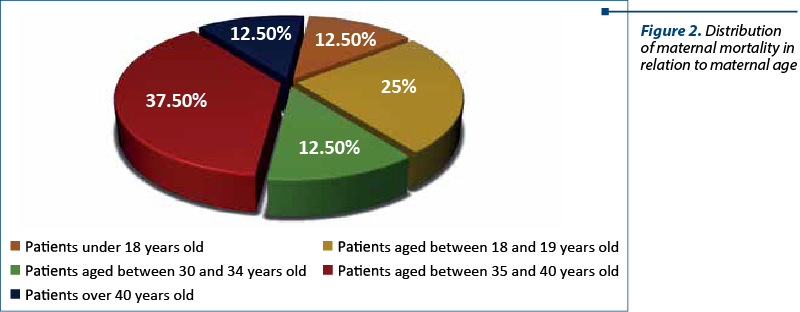
Concerning the maternal mortality registered in our study (n=8), the percentage recorded in the adolescent group was 37.5%, while in the control group the rate was 62.5%. The distribution of maternal mortality in relation to maternal age is presented in Figure 2.
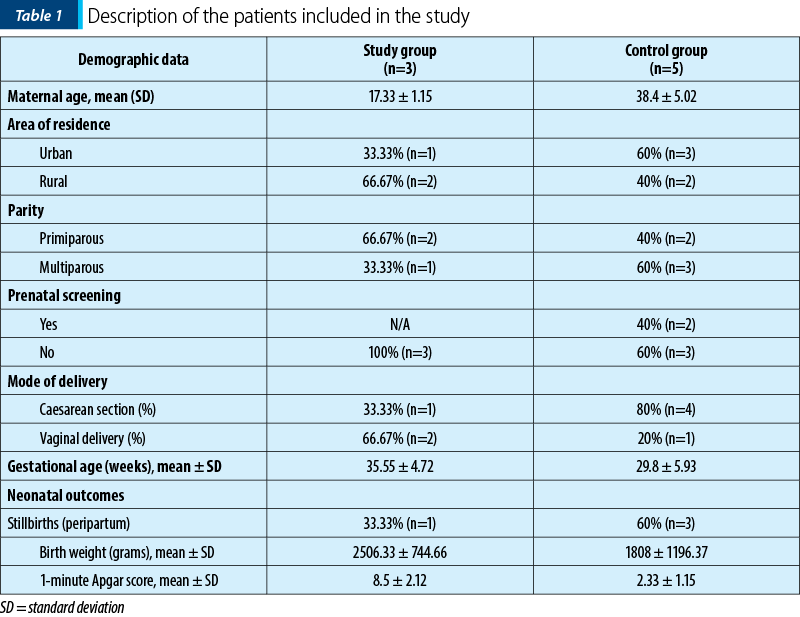
The two analyzed groups were divided according to maternal age, area of residence, parity, status of prenatal care, mode of delivery, gestational age and neonatal outcomes evaluated by stillbirth status, 1-minute Apgar score and birth weight (Table 1).
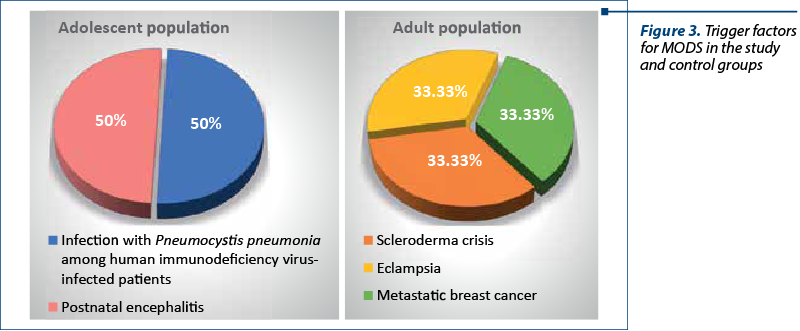
In the study group, the causes of death were: multiple organ dysfunction syndrome (66.67%, n=2) and brain death (33.33%; n=1). The causes of death among adult patients were, in the frequency order: multiple organ dysfunction syndrome (60%; n=3), and cardiogenic shock (40%; n=2). As presented, multiple organ dysfunction syndrome (MODS) was the most common cause of death in both groups, having an overall percentage of 62.5%. The trigger factors of MODS in the study and control groups are presented in Figure 3.
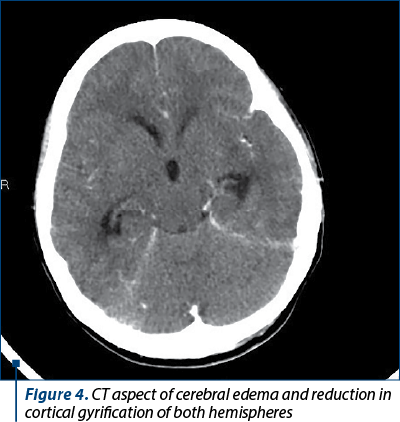
In the study group, a HIV-positive pregnant adolescent who had a preterm delivery at 30 weeks of pregnancy was diagnosed 14 days after admission with Pneumocystis pneumonia, the trigger for MODS. Another adolescent patient, who gave birth at term, was diagnosed with postnatal encephalitis three days after admission; after several neurosurgical interventions, the evolution was unpropitious (Figure 4). Regarding the patient with brain death, the trigger factor was sudden onset convulsive seizures which led to cerebellar tonsils herniation, the diagnosis being established upon presentation in our emergency room. After multiple investigations, the cerebral angiography described disrupted intracranial flow in bilateral cerebral arteries, which corresponded to cerebral death criteria (Figure 5).
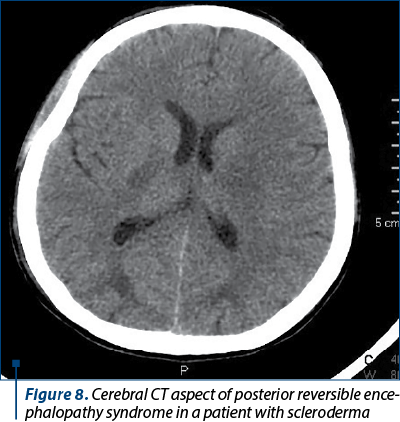
In the control group, the patients presented various determinant factors which led to death. Eclampsia led in one case to acute kidney injury and need of hemodialysis. Besides the eclampsia consequences, the patient had an uninvestigated renal pathology (nephrolithiasis) which favorized the sudden onset of renal dysfunction (Figure 6). The patient with breast cancer (mixed ductal and lobular carcinoma) had multiple metastases, including liver, vertebrae and lungs, therefore she had an accelerated unfavorable evolution (Figure 7). The patient with scleroderma was diagnosed with posterior reversible encephalopathy syndrome (PRES) 24 hours after delivery; the progression of scleroderma crisis was fulminant, resulting in maternal death (Figure 8). The determinant factors for the cardiogenic shock were endocarditis in one case, while in the other case the cause remained unknown.
Regarding the fetal prognosis, we registered 33.33% (n=1) of stillbirths in the group of adolescent patients. The reason of death was represented by placental dysfunction due to multiple maternal disorders. In the control group, the percentage of antepartum stillbirths was slightly increased (40%; n=2), the placental dysfunction due to eclampsia and cardiac pathology being the leading causes. In this group, we also registered an early neonatal death due to extreme prematurity (20%; n=1). Also, 66.67% of the newborns in the study group had a favorable prognosis, while in the control group the favorable outcome was registered in 40% of the cases.
The birth weight was significantly higher in the study group compared to the control group (2506.33±744.66 versus 1808±1196.37). The difference is correlated with gestational age (35.55 ± 4.72 versus 29.8±5.93), the high risk of preterm delivery in the second group being caused by patient’s underlying pathology (breast cancer, scleroderma crisis) or by pregnancy complications (eclampsia). The difference between the 1-minute Apgar score between the two groups (8.5±2.12 versus 2.33±1.15) had the same explanation: the prematurity translated by small gestational age at delivery in the control group (we did not register any case of fetal intrauterine restriction).



Discussion
In 2015, it was estimated that more than 303,000 women died due to complications associated to pregnancy and childbirth, and more than 90% of them occurred in low- and middle-income countries(23,24). In high-income countries, the rate of maternal death is estimated at 1 to 20 per 100,000 of those who give birth(25). In our department, between 30 September 2020 and 30 September 2022, the rate of maternal death was below 1%. Regarding maternal death among adolescents, most of the studies show that its incidence is higher in this population compared to the adult one(12-17). In our paper, the majority of patients declared dead after delivery were aged over 30 years old (62.5%), while adolescent mortality represented 37.5%.
The main classification of causes that lead to maternal death is comprised of direct and indirect factors. The direct ones refer to obstetrical complications such as interventions and pathological situations such as hemorrhage, obstructed labor, hypertension disorders or puerperal sepsis(26). The indirect causes of maternal deaths are represented by previously pathologies or pathologies developed during pregnancy which are aggravated during this period(26,27). In the study group, most of the causes of maternal death were represented by direct disorders such as eclampsia or postnatal encephalitis; only 33.33% were represented by HIV infection which was aggravated during pregnancy, being an indirect cause of death. In the control group, the results differ, as indirect causes of death are prevalent – scleroderma, breast cancer or endocarditis. Only 20% were direct causes of maternal death and the trigger was eclampsia. Previous research showed that adolescent patients have a higher risk of preeclampsia and eclampsia, followed by maternal death(16-19). In our study, the number of maternal deaths caused by eclampsia was similar in both groups, taking into consideration the case of convulsive seizures that took place in out-of-hospital environment and led to cerebellar tonsils herniation; this case had eclampsia as the most probable leading cause of death, taking into consideration that the patient had no history of epilepsy. Another point of view is that most of the studies compare adolescents with young adults, not with patients older than 34 years old, which also represent a group of risk for obstetrical complications(15-18).
Concerning the risk factors, inadequate antenatal care, hypertension disorders and delivery by caesarean section have been demonstrated to increase the risk of maternal mortality in any age(15,28). Furthermore, in the adolescent population, the risk of maternal death is higher due to low socioeconomic status, illiteracy or to disadvantaged area(12). In our work, we found that in the study group the majority of the patients were from rural area (66.67%), while in the control group this category was registered in only 40% of cases. Regarding the obstetrical characteristics, most of the adolescent patients were primiparous (66.67%) compared to the adult ones, where the percentage of primiparous patients was 40%. Regarding the mode of delivery, caesarean section was preponderant in the control group (80%), while in the study group, vaginal delivery was predominant (66.67%). These results confirm that the risk of maternal mortality is higher in the group of adult patients who underwent caesarean section, but it is not applicable to the adolescent group. Above all, the lack of antenatal care was 100% in adolescent patients and 60% in adult patients, confirming what previous works have revealed.
Regarding fetal death, an equal proportion of stillbirths was seen in both groups. A WHO multi-country study showed that stillbirth incidence is higher in adolescent mothers compared to patients aged between 20 and 24 years old, but also an increased risk is found in patients aged over 40 years old(29,30).
Study limitations. The small number of cases is one of the limitations of the study. Also, the gap of medical records and pregnancy data due to inadequate antenatal care are issues that limit the study.
Conclusions
Maternal mortality represents an important health problem, with various adverse impacts. Uninvestigated and severe pathologies may aggravate during pregnancy, as inadequate prenatal care predispose to a high risk of maternal and fetal mortality. Although the patients in our study have been evaluated and treated in a multidisciplinary hospital, the delayed time of admission was crucial for the negative prognosis. Therefore, adequate pregnancy medical controls and special programs for both adolescent and adult population may have a favorable result regarding the maternal and fetal mortality.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
-
Yazicioglu B, Yurtcu N, Guvey H, Caliskan CS, Celik S, Tinelli A. Perinatal and neonatal outcomes of adolescent pregnancies over a 10-year period. Ginekol Pol. 2022. Online ahead of print. https://pubmed.ncbi.nlm.nih.gov/36165639/
-
WHO. Adolescent pregnancy. Key facts. Available at: https://www.who.int/newsroom/fact-sheets/detail/adolescent-pregnancy
-
Pons-Duran C, Casellas A, Bardají A, Valá A, Sevene E, Quintó L, et al. Adolescent, pregnant, and HIV-infected: risk of adverse pregnancy and perinatal outcomes in young women from southern Mozambique. J Clin Med. 2021;10(8):1564.
-
Darroch J E, Woog V, Bankole A, Ashford LS. Adding it up: costs and benefits of meeting the contraceptive needs of adolescents. 2016. Available at: https://www.guttmacher.org/report/adding-it-meeting-contraceptive-needs-of-adolescents
-
WHO. Adolescents: health risks and solutions. 2018. Available at: https://www.who.int/news-room/fact-sheets/detail/adolescents-health-risks-and-solutions (accessed on Nov 14, 2022).
-
Azevedo WFD, Diniz MB, Fonseca ESVBD, Azevedo LMRD, Evangelista CB. Complications in adolescent pregnancy: systematic review of the literature. Einstein (São Paulo). 2015;13(4):618-26.
-
El Kazdouh H, El-Ammari A, Bouftini S, El Fakir S, El Achhab Y. Perceptions and intervention preferences of Moroccan adolescents, parents, and teachers regarding risks and protective factors for risky sexual behaviors leading to sexually transmitted infections in adolescents: qualitative findings. Reprod Health. 2019;16(1):138.
-
Unaids J. Fact sheet – latest global and regional statistics on the status of the AIDS epidemic. Geneva, UNAIDS, 2022. Available at: https://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf
-
Slogrove AL, Sohn AH. The global epidemiology of adolescents living with HIV: time for more granular data to improve adolescent health outcomes. 2018;13(3):170-8.
-
Chinsembu KC. Sexually transmitted infections in adolescents. Open Inf Dis J. 2009;3(1):107-17.
-
Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(9995):743-800.
-
Arias ESM, Cordero SJP, Mesa-Cano IC. Mortality rate and risk factors in adolescent pregnancy systemic review. Pro Sci. 2022;6(42):291-300.
-
Valencia MEF, Nava-Chapa G, Arenas-Monreal L. Adolescent pregnancy in Mexico: a public health issue. Rev Salud Publica (Bogota). 2017;19(3):374-8.
-
Bakwa-Kanyinga F, Valerio EG, Bosa VL, Alfama CO, Sperb M, Capp E, Vettorazzi J. Adolescent pregnancy: maternal and fetal outcomes in patients with and without preeclampsia. Pregnancy Hypertens. 2017;10:96-100.
-
Hayward G. Teenage pregnancy and its health implications. Int J Public Health Res. 2011;1(2):100-2.
-
Nove A, Matthews Z, Neal S, Camacho AV. Maternal mortality in adolescents compared with women of other ages: evidence from 144 countries. Lancet Glob Health. 2014;2(3):e155-64.
-
Blanc AK, Winfrey W, Ross J. New findings for maternal mortality age patterns: aggregated results for 38 countries. PLoS One. 2013;8(4):e59864.
-
Sullivan EA, Hall B, King JF. Maternal deaths in Australia, 2003-2005. Australian Institute of Health and Welfare. 2008. Available at: https://www.aihw.gov.au/getmedia/7eee0f5e-ecec-48d6-a291-c9c13ad0184d/mdia03-05.pdf.aspx?inline=true
-
Conde-Agudelo A, Belizán JM, Lammers C. Maternal-perinatal morbidity and mortality associated with adolescent pregnancy in Latin America: Cross-sectional study. Am J Obstet Gynecol. 2005;192(2):342-9.
-
Teenage pregnancy/report by the Social Exclusion Unit; presented to Parliament by the Prime Minister by command of Her Majesty, 1999. Available at: https://wellcomecollection.org/works/nfyxxux5
-
DeMarco N, Twynstra J, Ospina MB, Darrington M, Whippey C, Seabrook JA. Prevalence of low birth weight, premature birth, and stillbirth among pregnant adolescents in Canada: a systematic review and meta-analysis. J Pediatr Adolesc Gynecol. 2021;34(4):530-7.
-
Centers for Disease Control and Prevention: What is stillbirth? Available at: http://www.cdc.gov/ncbddd/stillbirth/facts.html. (Accessed Nov 14, 2022).
-
Merdad L, Ali MM. Timing of maternal death: levels, trends, and ecological correlates using sibling data from 34 sub-Saharan African countries. PLoS One. 2018;13(1):e0189416.
-
WHO, UNICEF, UNFPA, World Bank Group, United Nations Population Division. Trends in maternal mortality: 1990 to 2015. Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division; 2015, Geneva: WHO. Available at: http://apps.who.int/iris/bitstream/10665/194254/1/9789241565141_eng.pdf?ua=1.
-
Neggers YH. Trends in maternal mortality in the United States. Reprod Toxicol. 2016;64:72-6.
-
Mekonnen W, Gebremariam A. Causes of maternal death in Ethiopia between 1990 and 2016: systematic review with meta-analysis. Ethiopian J Health Develop. 2018;32(4):225-42.
-
IDC 10. International Statistical Classification of Diseases and related health problems. WHO, Geneva. Available at: https://apps.who.int/iris/bitstream/handle/10665/42980/9241546530_eng.pdf?sequence=1&isAllowed=y
-
Bauserman M, Lokangaka A, Thorsten V, Tshefu A, Goudar SS, Esamai F, Bose CL. Risk factors for maternal death and trends in maternal mortality in low-and middle-income countries: a prospective longitudinal cohort analysis. Reproductive Health. 2015;12(2):1-9.
-
Noori N, Proctor JL, Efevbera Y, Oron AP. Effect of adolescent pregnancy on child mortality in 46 countries. BMJ Glob Health. 2022;7(5):e007681.
-
Ganchimeg T, Ota E, Morisaki N, Laopaiboon M, Lumbiganon P, Zhang J, WHO Multicountry Survey on Maternal Newborn Health Research Network. Pregnancy and childbirth outcomes among adolescent mothers: a World Health Organization multicountry study. BJOG. 2014;121 Suppl 1:40-8.
Articole din ediţiile anterioare
Implicaţii şi consecinţe ale sarcinii la adolescente
Context. Numărul sarcinilor în rândul adolescentelor este în continuă creştere la nivel global, ca urmare a schimbărilor sociale şi libertăţii sexu...
Complicaţii rare pe termen lung ale intervenţiilor minim invazive în cursul sarcinii
Introducere. Procedurile ginecologice minim invazive, precum miomectomia histeroscopică sau laparoscopică şi rezecţia histeroscopică a septurilo...
Sindromul vanishing twin şi impactul său perinatal - review al literaturii de specialitate
Folosirea pe scară largă a tehnicilor de reproducere umană asistată a dus la creşterea numărului de sarcini gemelare sau multiple. Asociat cu acest...
Profesia de moaşă, între tradiţie şi modernism
Necesitatea reconsiderării acestei profesii este impusă şi de datele statistice care clasează România pe primele locuri în Europa în ceea ce priveş...