The most frequently used tools to differentiate between a normal pregnancy and an ectopic or nonviable one are human chorionic gonadotropin concentration and high-resolution transvaginal ultrasound measurements. Extensive prenatal ultrasound, using a wide range of criteria, can be used to identify pregnancies at risk for the mother or fetus, ensuring an ongoing evaluation of the maternal and fetal health and anticipating certain problems that allow in some cases to minimize or even prevent morbidity. The specialist must first determine the viability of the pregnancy, the localization, the number of sacs, embryos, placentas and, after all these, the gestational age. The most used signs for early pregnancy failure are considered the absence of cardiac activity and the absence of the embryo in a grown gestational sac. Beside ultrasonography, hCG levels are used to differentiate between viable pregnancies, nonviable pregnancies and ectopic pregnancies, even though values overlap most of the time, as a result multiple measurements must be performed. When the last menstrual period is not known, ultrasonography can be used to date the pregnancy using ultrasound measurements. Ultrasonography can be used to detect congenital anomalies during early pregnancies, as well as detect first-trimester fetal growth delay. Currently, there is a constant need of revising and standardizing the practical guidelines with the purpose of ensuring that patients receive the best prenatal care as possible, as well as treating the nonviable during the first trimester at low costs, preventing further costs down the road.
Criteriile ultrasonografice ale viabilităţii şi neviabilităţii sarcinii incipiente
Early pregnancy signs of viability and failure
First published: 17 noiembrie 2021
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.34.4.2021.5694
Abstract
Rezumat
Cel mai frecvent folosite investigaţii pentru a diferenţia o sarcină normală de o sarcină neviabilă sau de o sarcină ectopică sunt gonadotropina corionică umană şi măsurătorile ecografice transvaginale de înaltă rezoluţie. Ecografiile prenatale extensive, folosind un număr suficient de criterii, pot fi utilizate la identificarea sarcinilor la risc pentru mamă şi făt, pentru asigurarea unei evaluări continue a sănătăţii mamei şi fătului, cu scopul de a anticipa posibilele probleme şi pentru a permite, în unele cazuri, scăderea sau chiar prevenirea morbidităţii. Medicul trebuie în primul rând să determine viabilitatea sarcinii, localizarea acesteia, numărul sacilor gestaţionali, al embrionilor, placentelor şi, după toate acestea, vârsta gestaţională. Cele mai utilizate semne pentru sarcina neviabilă în primul trimestru sunt absenţa activităţii cardiace şi absenţa embrionului într-un sac gestaţional normal. În afara ecografiei, nivelul beta-HCG-ului este folosit pentru a diferenţia între sarcina normală, cea neviabilă şi cea ectopică, chiar dacă nivelurile de beta-HCG se suprapun în diferite momente, având drept consecinţă nevoia de măsurători în dinamică. Atunci când data ultimei menstruaţii nu este cunoscută, ultrasonografia poate fi folosită pentru a data sarcina cu ajutorul măsurătorilor. Ultrasonografia poate fi utilizată pentru a detecta defecte congenitale în sarcina incipientă sau pentru a detecta restricţii de creştere în primul trimestru. În prezent, există o nevoie constantă de revizuire şi standardizare a ghidurilor clinice, cu scopul de a le oferi pacientelor cel mai înalt standard de servicii medicale, alături de posibilitatea de a trata sarcina neviabilă în primul trimestru, cu costuri mici, prevenind cheltuielile ulterioare.
Introduction
In today’s obstetrics, the early diagnosis of pregnancy is of a high importance. Since over three decades ago, ultrasonography – especially transvaginal ultrasonography – represents the elective method to make the differential diagnosis and management of viable, ectopic and nonviable pregnancies, markedly reducing the morbidity and mortality associated with ectopic pregnancy.
Transvaginal ultrasonography still has criteria with almost 100% specificity for nonviable pregnancies, which leads to an important decrease in costs regarding future examinations. Considering the increase of pregnancies inserted on the post-caesarean surgery scar and the efficiency of the treatment methods available for ectopic or nonviable pregnancies diagnosed in early first trimester, we consider that performing an ultrasonographic evaluation for pregnancy confirmation between 6 and 9 weeks of amenorrhea is extremely important and must be available, within health insurance, for all women with amenorrhea and a positive pregnancy test, no matter their risk group, but mainly for those with a history of caesarean section births, conservative uterine surgeries and ectopic pregnancy(1).
As the medical technology and tools available advance more and more towards a very high standard of treatment, there is less room for error than ever. Errors in discerning between a viable intrauterine pregnancy and nonviable/ectopic pregnancy are a major starting point for a high number of malpractice lawsuits(2).
The majority of practitioners use for the diagnosis and management of incipient pregnancies the serum concentration of human chorionic gonadotropin and transvaginal ultrasonography. The Romanian Society of Obstetrics and Gynecology (SOGR), as of 2019 guidelines, recommends the early confirmation of pregnancy between 6 weeks and 9 weeks of gestation and a further first-trimester ultrasound examination of fetal anatomy at 11-13+6 weeks(2). The American College of Obstetricians and Gynecologists (ACOG) and the American Institute of Ultrasound in Medicine (AIUM) recommend the ultrasound examination for all pregnant patients, no matter their associated class of risk. Furthermore, the American guidelines recommend screening ultrasound examination for the detection of fetal abnormalities and other possible complications of pregnancy(3).
In order to correctly assess the pregnancy, the specialist must first determine the viability of the pregnancy, the localization, the number of sacs, embryos, placentas and, after all these, the gestational age, which is fundamental in order to compare the obtained parameters during examinations with the standard charts(1).
In the majority of guidelines, the diagnosis of pregnancy is confirmed by:
a. The detection of human chorionic gonadotropin (hCG) in blood or urine (blood test is more reliable as it has a lower threshold for a positive test).
b. The identification of pregnancy by ultrasound.
The next step after confirming the pregnancy is to determine whether the pregnancy is intrauterine or ectopic and if the pregnancy is viable or nonviable, which is done using hCG and ultrasonography. Ultrasonography is a pivotal point in the management of every pregnancy, used from the beginning until the very end. Over time, a series of criteria were developed to monitor the normal evolution of a pregnancy. By comparing the measurements with the standards, pregnancies can be separated in viable and nonviable, or we can identify a growth delay.
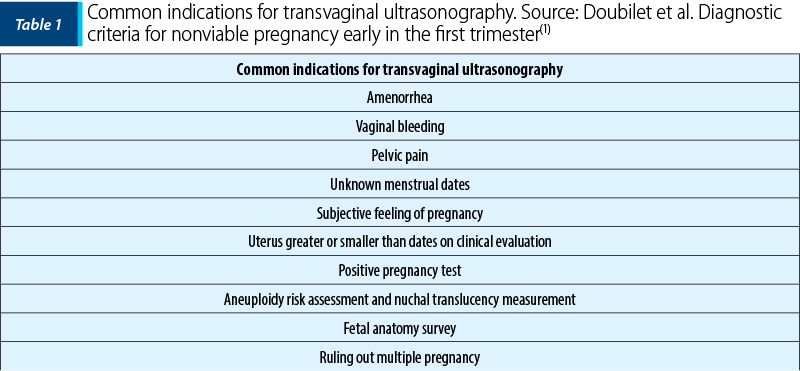
Although there are many opinions regarding the indications of early first-trimester ultrasound (Table 1), we consider it indispensable in order to confirm an intrauterine gestation, to accurately date the pregnancy, to assess the number and viability of the embryos, to diagnose major fetal malformations and, most important, to detect any early markers of pregnancy failure.
Ultrasonographic signs for early pregnancy failure in intrauterine pregnancy
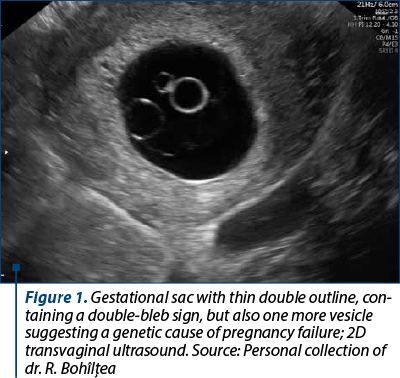
The most used signs for early pregnancy failure (Figure 1) are considered the absence of cardiac activity and the absence of the embryo in a grown gestational sac. None of these signs have a 100% specificity or sensitivity and measurements for the same patient can differ from one device to another or from one practitioner to another.
A. Crown Rump Length (CRL) criteria for failed pregnancy – recent studies have shown that a cutoff of 7 mm for a CRL with no cardiac activity to be as close as possible to 100% specificity; if the practitioner finds no cardiac activity in an embryo between 5 (older cutoff value used which led to a significant number of false-positive failed pregnancies) to 7 mm, there is a suspicion of failed pregnancy and not a diagnostic failure(1).
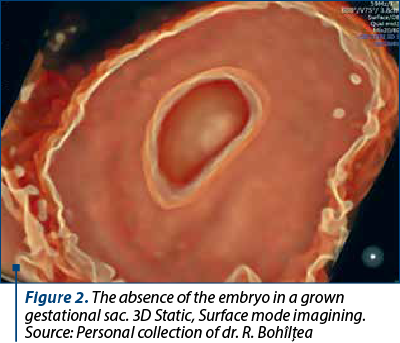
B. Mean Sac Diameter (MSD) criteria for failed pregnancy – the MSD is obtained by measuring the sagittal, transverse and anteroposterior diameter of the sac. The first cutoff suggested for practical use was 16 mm (the point at which the embryo is visible in the sac), which was later changed to 25 mm as many 17 to 21 mm gestational sacs with no embryo, considered nonviable, would later turn to be viable pregnancies (Figure 2). As a result, nowadays we use a cutoff of 25 mm for the MSD with no embryo visible to identify a nonviable pregnancy(1).
C. Time-based criteria for failed pregnancy – some pregnancies fail even before we are able to identify the gestational sac or to be able to identify the embryo and measure it, so the need arise for other criteria to be established. As such, not being able to see an embryo with heartbeat by a certain point in time (after six weeks) is predictive enough for a failed pregnancy. Other more specific and sensitive criteria are based on combining a series of ultrasound scans and timing events of early pregnancy like the appearance of gestational sac and yolk sac. Currently, the most reliable time-based criteria for failed pregnancies are an embryo with no heartbeat more than two weeks after a scan that confirmed a gestational sac and an embryo with no heartbeat more than 11 days after a scan confirmed a gestational sac with a yolk sac(1).
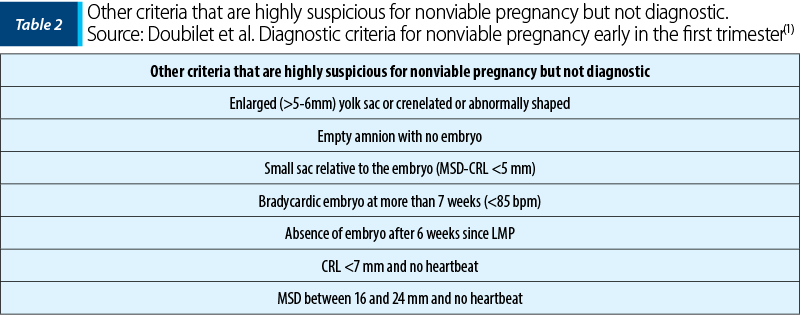
D. Other criteria that are highly suspicious for nonviable pregnancy but not diagnostic (Table 2) – these abnormalities are derived from previous criteria and practically represent the gray area in which some pregnancies turn out to be nonviable while others turn out to be viable(1).
The most recent study on topic was published last month in the White Journal by Dooley et al. and conducted by D. Jurkovic(4). The study included 6012 women with early pregnancy complications, being the largest study sustaining that the finding on ultrasound of an amniotic sac without an embryo with cardiac activity, named “amniotic sac sign”, is a reliable marker of early pregnancy failure, able to reduce the number of follow-up scans by 11%(4).
Pregnancies with unknown location – possible scenarios and how to diagnose nonviable pregnancies
An important part in managing these scenarios (Figure 3) is the measurement of hCG. Human chorionic gonadotropin is a hormone created primarily by the syncytiotrophoblast cells of the placenta which is produced in early pregnancy. Its main role is to stimulate the corpus luteum to produce progesterone in order to maintain the pregnancy. The hCG is produced mainly in the first trimester, reaching a peak around the 10th pregnancy week, after which it decreases and enters a plateau phase until delivery (Figure 4). After delivery, the hCG levels return to the normal range in between one week and two months. During the first two months of pregnancy, the concentration doubles every 24 to 48 hours and it reaches a detectable level in serum at 1 to 2 mIU/mL and 20 to 50 mIU/mL in urine tests, corresponding to the 4th week of pregnancy(5).
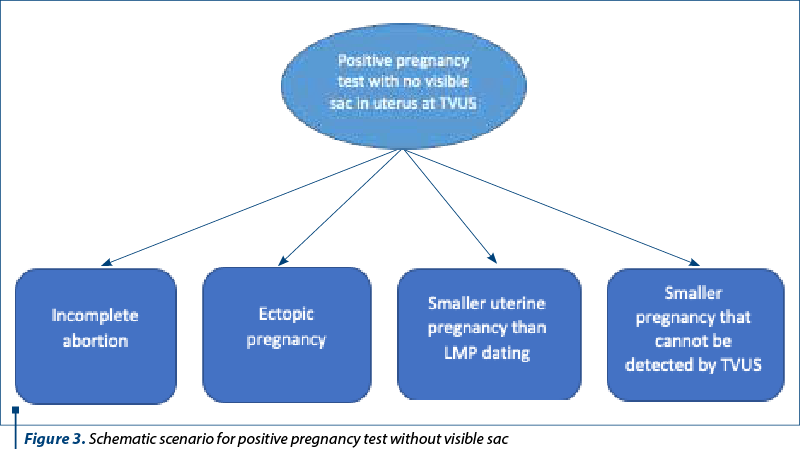
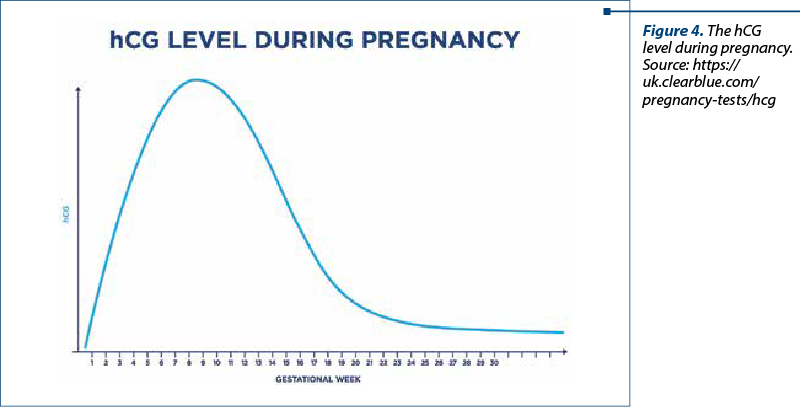
Although hCG levels in viable pregnancies, nonviable pregnancies and ectopic pregnancies overlap most of the time, multiple measurements must be performed. Modern ultrasonography can detect a gestational sac at around 1000 to 2000 mIU/ml. A viable pregnancy doubles its hCG every two days and therefore at least two measurements at the same laboratory are required. For a woman with unknown pregnancy location with a hCG level of 2000-3000 mIU/ml, the ectopic pregnancy is 19 times more likely, while a nonviable intrauterine pregnancy is 38 times more likely(1).
In order to confirm a viable pregnancy, the hCG is evaluated every two days. If the doubling pattern is not respected, the pregnancy is considered nonviable. A concentration of hCG that is slowly rising is suggestive for an ectopic pregnancy which requires further ultrasonography for confirmation. A decrease in the concentration of hCG is suggestive for abortion, incomplete abortion or tubal abortion. Other high-risk factors for ectopic pregnancy must be evaluated through history like previous ectopic pregnancy, tubal surgery or pathology, in vitro fertilization or intrauterine devices(5,6).
Assessment of gestational age
and correlations with hCG level
The precise determination of gestational age, although easy in theory, can be a real challenge. The most frequent sign is amenorrhea, which in patients with irregular menses is not a very reliable symptom. In addition, spotting or bleeding can occur in around 10-15% of women during early pregnancies, which tends to overlap with the last menstrual period, giving the false impression of nonpregnancy. When the last menstrual period is not known, ultrasonography can be used to date the pregnancy using ultrasound measurements (Figure 5)(7,8).
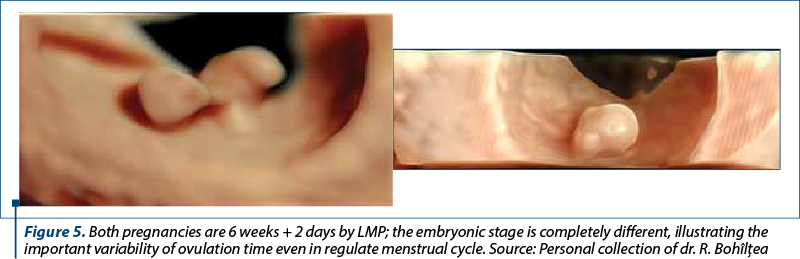
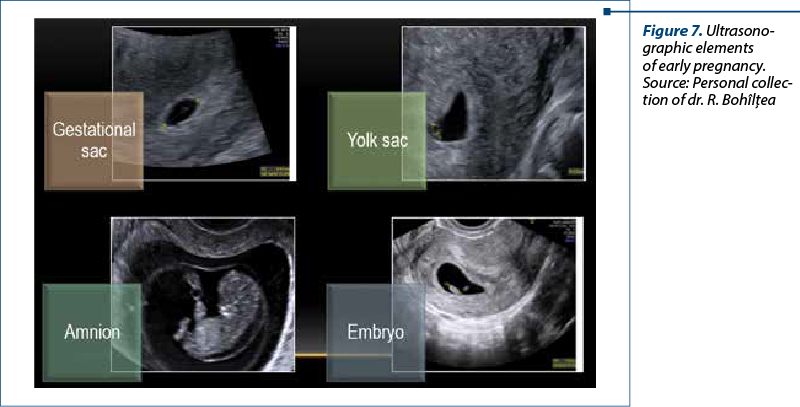
The first element that can be identified by transvaginal ultrasonography in a pregnancy is the gestational sac which can be found four to four and a half weeks after conception. It appears as a round or later elliptic sac filled with fluid with a thick, hyperechogenic contour. The lowest threshold at which it can be spotted is 2 to 3 mm. The change of form from round to irregular might be a sign for a failed pregnancy(1,7).
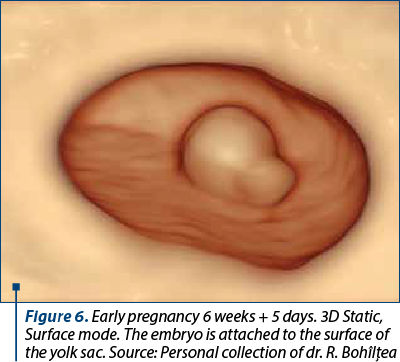
After five weeks of amenorrhea, the first anatomic structure that can be seen inside the gestational sac (which at this point is around 5 mm) is the yolk sac (Figure 6). It is a spherical structure with an echogenic periphery that continues to grow up until the 10th week when it reaches 6 mm. After this period of growth, the yolk sac migrates to the periphery of the sac and it becomes unidentifiable by the end of the first trimester. The diameter of yolk sac can be used to identify abnormal pregnancies(7).
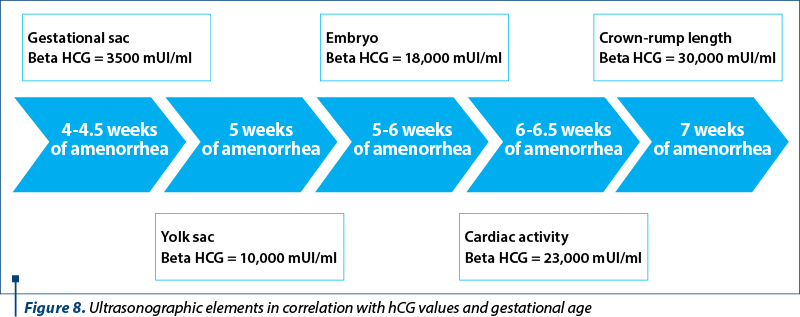
The embryonic disk is visible from 1 to 2 mm, which corresponds to a gestational age of 5 to 6 weeks. As the pregnancy progresses, the gestational sac and yolk sac lose their accuracy for estimating gestational age. Between the 6th and the 10th weeks of pregnancy, the amniotic sac follows the embryonic development (Figures 7 and 8)(7). When the embryo reaches at least 5 mm, the cardiac activity can be seen using transvaginal ultrasonography. The presence of cardiac activity after 6 weeks is a central element in establishing if a pregnancy is viable or nonviable. The heart rate increases quickly from 100 beats per minute at 6 weeks of gestation to 145-170 beats per minute at 8 weeks and to180 beats per minute at 10 weeks, after that it decreases and plateaus at an average of 140 beats per minute(7).
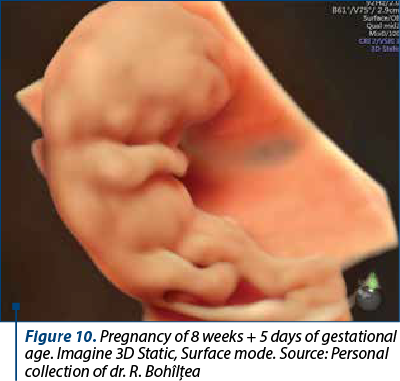
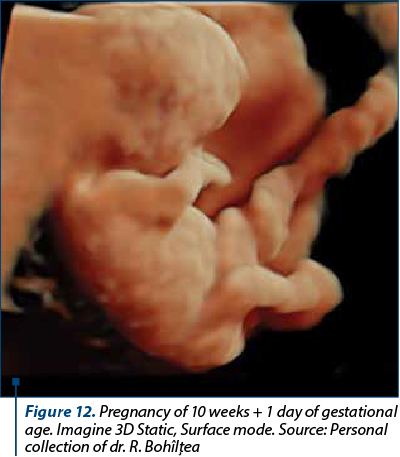
From the 7th week of pregnancy, the most useful measurement to assess the gestational age is the crown rump length (CRL). It is used to evaluate the development of the embryo and to correct the gestational age if there is a gap of more than 5 days between the last menstrual period and CRL before 9 weeks and a gap of more than 7 days between 9 to 14 weeks (Figures 9-14)(9).
First-trimester fetal growth delay
The early fetal growth delay was observed to be predictive of subsequent adverse perinatal outcomes. Embryos usually grow by 1 mm per week between the 6th and the 9th weeks of gestation. As such, a lag in CRL growth during the first trimester is suggesting a delay rather than an incorrect dating of the pregnancy(10).




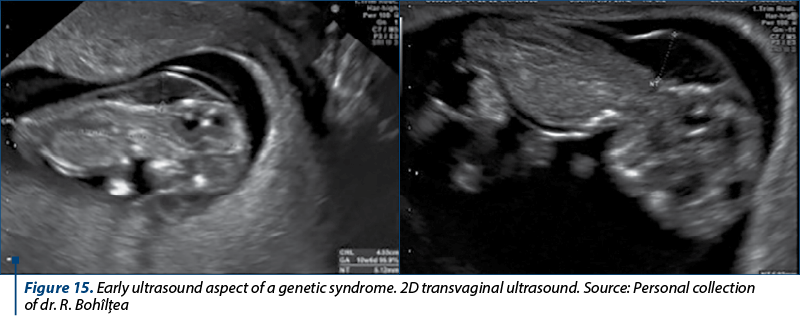
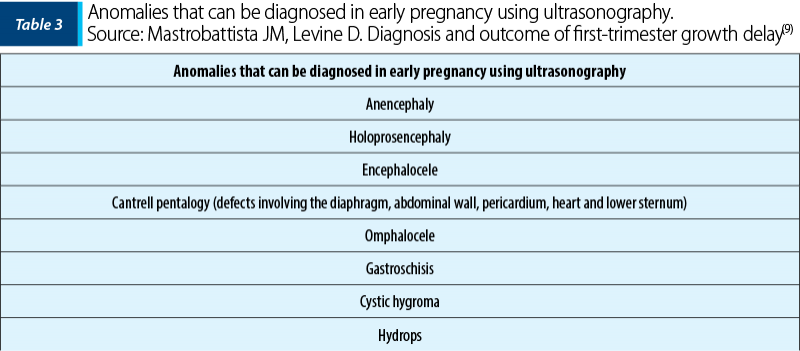
Possible etiologies (Table 3) for the delay could be aneuploidy, congenital anomalies (Figure 15), suboptimal uterine environment or constitutional factors. Studies found out that a CRL deficit is associated with a high risk of failed pregnancy, preterm or low birth weight and with a high cardiovascular risk(10).
If present, first-trimester fetal growth delay is an indication for an early survey of fetal anatomy. The further assessment of fetal anatomy should be performed between the 18th and the 20th weeks, or earlier if possible(10).
Conclusions
It is necessary to create and promulgate widely guidelines for practitioners involved in the diagnosis and management of problems in early pregnancy, in order to improve patient care and reduce the risk of inadvertent harm to potentially normal pregnancies.
Higher rates of caesarean section births and more frequent conservative uterine surgeries led to an increase in invasive pregnancies on the resulting scars. If diagnosed early, not only it is treatable at lower costs and without consequences, but it reduces costs and, more importantly, the morbidity and mortality.
Recent studies have introduced a series of criteria based on fetal measurements and laboratory tests that, used together, have a very high specificity and sensibility which minimize the risk of false-positive results.
Conflicts of interests: The authors declare no conflict of interests.
Bibliografie
SOGR. Ghiduri clinic de obstetrică-ginecologie din 2019 până în prezent, chapter 1 and chapter 17. Available at: https://sogr.ro/ghiduri-clinice-2019-prezent-1/
AIUM practice guideline for the performance of obstetric ultrasound examinations. J Ultrasound Med. 2013;32(6):1083-101.
Dooley WM, Braud LDE, Thanatsis N, et al. The predictive value of presence of amniotic sac without visible embryonic heartbeat in diagnosis of early embryonic demise. Ultrasound Obstet Gynecology. 2021;57:149-54.
Betz D, Fane K. Human Chorionic Gonadotropin. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2021 Jan. Available at: https://www.ncbi.nlm.nih.gov/books/NBK532950/
Bastian LA, Brown HL. Clinical manifestations and diagnosis of early pregnancy. UpToDate. Available at: https://www.uptodate.com/contents/clinicalmanifestations-and-diagnosis-of-early-pregnancy
MacKenzie AP, Stephenson CD, Funai EF. Prenatal assessment of gestational age. UpToDate. Available at: https://www.uptodate.com/contents/prenatal-assessment-of-gestational-age-date-of-delivery-andfetal-weight
Harville EW, Wilcox AJ, Baird DD, Weinberg CR. Vaginal bleeding in very early pregnancy. Hum Reprod. 2003;18(9):1944-7.
Lockwood CJ, Magriples U. Prenatal care: initial assessment. UpToDate. Available at: https://www.uptodate.com/contents/prenatal-care-initial-assessment
Mastrobattista JM, Levine D. Diagnosis and outcome of first-trimester growth delay. UpToDate. Available at: https://www.uptodate.com/contents/diagnosisand-outcome-of-first-trimester-growth-delay
Articole din ediţiile anterioare
Complicaţii materne şi neonatale în sarcina gemelară obţinută spontan versus sarcina gemelară obţinută prin FIV
Acest studiu a avut ca obiectiv identificarea complicaţiilor materne şi neonatale din sarcina gemelară obţinută spontan, comparativ cu sarcina gem...
Riscurile pentru sănătatea mamei în cazul sarcinilor la vârste extreme
Introducere. Patologiile asociate sarcinilor la vârste extreme au implicaţii clinice potenţiale semnificative atât asupra stării de sănătate a mam...
Evaluarea clinică şi ecografică a feţilor şi a anexelor fetale la gravidele cu trombofilii ereditare
Statutul de pacientă gravidă presupune o stare de hipercoagulabilitate, cu scopul de a pregăti viitoarea mamă pentru momentul naşterii. Atunc...
Impactul psihoemoţional al sarcinii ectopice – experienţa clinicii noastre
Introducere. Studiul de faţă a avut drept scop identificarea şi evaluarea impactului psihoemoţional al femeilor care au fost diagnosticate cu sarci...