Background. Schizophrenia is a public health burden and a severe type of mental disorder that has a significant distress to the individual and the society. Pharmacotherapy is the mainstay of the treatment, and the rational prescription is guided by World Health Organization (WHO) prescribing indicators developed to assess pharmaceutical prescribing practices by health providers. This study evaluated the pattern of health providers’ prescription of psychotropic drugs for schizophrenia patients from a tertiary mental health facility in Anambra State, southeastern part of Nigeria. Methodology. This was a one-year retrospective, descriptive, cross-sectional study of psychotropic medicines prescriptions for adult schizophrenia patients who were at least 18 years old, to assess the average number of drugs prescribed per encounter, the percentage of encounters with injection prescribed, the percentage of drugs prescribed by generic name, and the percentage of drugs prescribed from the Essential Medicines List. Results. A total of 338 encounters were assessed after random sampling, and the results show that the average number of prescriptions per encounter was 3.23, while 95.97% of the total number of drugs were prescribed by generic names, in 26.9% of the total number of encounters there were prescribed injections, while 100% of the prescribed drugs were from the Essential Medicines List. Other indicators reveal that fluphenazine was the most prescribed antipsychotic injection, while haloperidol and olanzapine were the most prescribed typical and atypical antipsychotics, respectively. Conclusions. There were issues of polypharmacy, some reluctance in prescribing drugs with generic names, and overuse of injections.
Prescription pattern of psychotropic medicines for patients with schizophrenia in a tertiary hospital of southeast Nigeria
Tipare de prescriere a psihotropelor pentru pacienţii cu schizofrenie dintr-un spital terţiar din sud-estul Nigeriei
First published: 23 aprilie 2024
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Psih.76.1.2024.9467
Abstract
Rezumat
Context. Schizofrenia este o povară pentru sănătatea publică şi un tip sever de tulburare mintală, cu un impact semnificativ asupra individului şi societăţii. Farmacoterapia este baza tratamentului, iar prescrierea raţională este ghidată de indicatorii de prescriere ai Organizaţiei Mondiale a Sănătăţii (OMS), dezvoltaţi pentru a evalua practicile de prescriere farmaceutică de către furnizorii de sănătate. Acest studiu a evaluat modelul de prescriere a medicamentelor psihotrope pentru pacienţii cu schizofrenie dintr-o unitate terţiară de sănătate mintală din statul Anambra, partea de sud-est a Nigeriei. Metodologie. Acesta a fost un studiu retrospectiv, descriptiv, transversal, pe o perioadă de un an, privind prescrierea medicamentelor psihotrope la pacienţii adulţi cu schizofrenie, cu vârsta de cel puţin 18 ani, pentru a evalua numărul mediu de medicamente prescrise per întâlnire, procentajul de consultaţii în urma cărora au fost prescrise injecţii, procentajul de medicamente prescrise cu denumirea generică şi procentajul de medicamente prescrise din Lista Medicamentelor Esenţiale. Rezultate. Un total de 338 de consultaţii au fost evaluate după eşantionarea aleatorie, iar rezultatele arată că numărul mediu de prescrieri per întâlnire a fost de 3,23, în timp ce 95,97% din numărul total de medicamente au fost prescrise cu denumirea generică, în 26,9% din numărul total de întâlniri au fost prescrise injecţii, în timp ce 100% din medicamentele prescrise au fost din Lista Medicamentelor Esenţiale. Alţi indicatori relevă că flufenazina a fost cel mai prescris antipsihotic injecabil, în timp ce haloperidolul şi olanzapina au fost cele mai prescrise antipsihotice tipice şi, respectiv, atipice. Concluzii. Au fost constatate unele probleme legate de polifarmacie, câteva cazuri de reticenţă în prescrierea medicamentelor cu denumiri generice, alături de utilizarea excesivă a formelor injectabile.
1. Introduction
1.1. Background of the study
Schizophrenia is a public health burden and a severe type of mental disorder which has a significant distress to the individual, close relatives and the society at large. Moreover, the global situation of mental disorders seems be worrisome since the prevalence has tripled after the COVID-19 pandemic, making close to 1 billion people struggling with the condition, whereas about 82% of them are in low- and middle-income countries(1).
Nigeria, a lower middle-income country, which is the seventh largest country in the world and the most populous in Africa, with more than 200 million people, is reported to have about one in every four persons with a mental illness, accounting for more than 50 million sufferers of mental disorders(2). However, the prevalence of schizophrenia is low (about 0.4%), but the illness is severe compared with other mental illnesses(3). This group of patients is two or three times more likely to die early in life, probably due to physical illnesses. Whereby as much as 50% of patients in neuropsychiatric hospitals are diagnosed, only 31.3% receive specialist mental healthcare(4), whereas a substantial proportion of them are left to cope by themselves(5). In situations where the conditions of the patients are not properly managed, it can lead to their inability to perform meaningful tasks and to lower contributions to the society(5).
Pharmacotherapy remains the mainstay of treatment in patients with schizophrenia, and psychotropic medication prescriptions are guided by prescription indicators that were developed by World Health Organization (WHO) to assess areas that include pharmaceutical prescribing practices by healthcare providers(6). However, there are limited data to show the compliance of the prescribers, considering the recommended prescription guidelines.
Hence, this study evaluated the pattern of prescriptions of psychotropic drugs for schizophrenia patients who visit a tertiary mental health facility in Anambra State, southeastern part of Nigeria. It specifically assessed the commonly used psychotropic medicines, the trends, and their extent of rational use in schizophrenia patients.
2. Methodology
2.1. Study site and study setting
The study was conducted at the Anambra State Neuropsychiatric Hospital, Nawfia, in the southeastern part of Nigeria. The hospital is located on the Enugu-Onitsha old express way, about 4 km from the state capital and about 30 km from the state commercial city center. The hospital has been providing psychiatric services since its establishment in 1991 by the government. In 2023, it had a total of 38 beds, with about 90% to 100% steady occupancy, and the staff was represented by 93 specialists: physicians, pharmacists, nurses, other healthcare professionals, and the support staff. More than 95% of the daily visitors are outpatients that come to fill prescription or visit the physicians for treatment or counseling. The hospital structure consists of: general outpatient department (one), dispensary (two), chief pharmacist office (one), physicians consulting offices (three), medical laboratory (one), medical records office (one), male wards (one for acute patients, one for recovery), female wards (one for acute patients, one for recovery), staff general office (one), and students’ hostel (one).
2.2. Study design
This was a one-year (from the 1st of April 2022 to the 31st of March 2023) retrospective, descriptive, cross-sectional study of psychotropic medicines prescriptions for adult schizophrenia patients who were at least 18 years old and visited the hospital.
2.3. Data collection
A standardized drug use indicators to investigate drug use in healthcare facilities(6) was employed. According to the report by the hospital health information unit, there were a total of 8321 encounters for various mental disorders. Out of the total number, there were 698 encounters of adult patients with only schizophrenia that were eligible for the study. The prescription records, which contained the patients’ names, ages, gender and the prescribed drugs, were kept manually in the pharmacy unit. Relevant data were collected using a designed prescribing indicator form which contained questions on age, sex, number of drugs per encounter, drugs prescribed by generic name, injection(s) prescribed, and drugs prescribed from the Essential Medicines List. The prescribing indicators were adopted from WHO selected drug use indicators to investigate drug use in healthcare facilities(6). We evaluated the average number of drugs prescribed per encounter, the percentage of encounters with injection prescribed, the percentage of drugs prescribed by generic name, and the percentage of drugs prescribed from the Essential Medicines List. The WHO core indicators were assessed as follows:
i) Average number of drugs prescribed per encounter = total number of drugs prescribed/total number of encounters surveyed.
ii) Percentage of encounters with an injection prescribed: the number of patient encounters with an injection prescribed/total number of encounters surveyed × 100.
iii) The percentage of drugs prescribed by generic names is expected to be 100%.
iv) Percentage of drugs prescribed from the Essential Medicines List: number of products prescribed from the Essential Medicines List/total number of products prescribed × 100%.
The period of data collection was from the 24th of September 2023 to the 6th of November 2023.
2.4. Eligibility criteria
2.4.1. Inclusion criteria:
-
Psychotropic medication prescriptions for confirmed diagnosis of schizophrenia spectrum.
-
Prescriptions for patients with ages from 18 to 65 years old.
2.4.2. Exclusion criteria:
-
Prescriptions for affective disorders.
-
Prescriptions of clear experience of more than one discrete psychotic episode.
-
Prescriptions for those on clozapine who require close monitoring.
2.4.3. Sample size determination/ sampling technique
Sample size calculation for a finite population:
S = X²NP (1-P) ⁄d² (N-1) + X²P (1-P)(7)
Where:
X = 1.96 (Z value for 95% confidence interval).
N = 698 (population size).
P = 0.5 (50% population proportion).
d = 0.05 (degree of accuracy/margin of error).
Sample size =
1.96²×698×0.5(1-0.5) ⁄0.05²(698-1) + 1.96²×0.5(1-0.5)
=
3.8416×698×0.5(0.5) ⁄0.0025(697) + 3.8416×0.5(0.5)
= 670.4⁄ 2.7
= 248.
Allowing for 10% drop out rate accounted to a minimum sample size of 273.
Although the minimum number of patients’ prescription needed to be reviewed in a single healthcare facility for more reliable results according to World Health Organization is 100(8), a systematic random sampling was employed to collect the data from every second prescription of 698 encounters of schizophrenia patients in order to give a more reliable result.
2.5. Data analysis
Data were analyzed with the use of designed Excel worksheet to collect relevant data based on indicators. The data collected were transferred into Excel spreadsheet and analyzed for prescriptions by the number of prescription of drugs by generic names versus brand names, theproportion of prescribed injections, and theproportion of prescriptions from the Essential Medicines List. Other used indicators collected and analyzed were prescriptions by gender and the proportion of the patients’ ages.
2.6. Ethical considerations
A study code for the purpose of data was used to ensure the confidentiality of information. Ethical clearance was obtained from the hospital ethics committee (Ref: NPHN/010). The researcher was made aware that the research process can be terminated if he/she was not following the study protocol.
3. Results
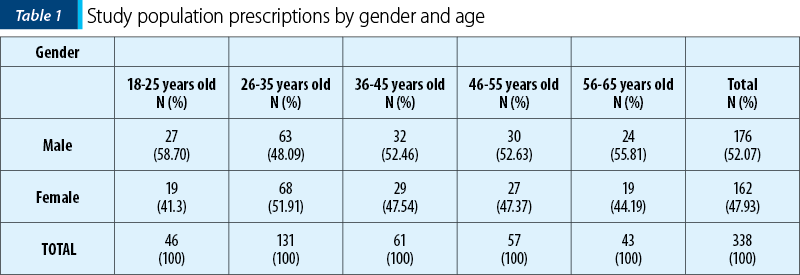
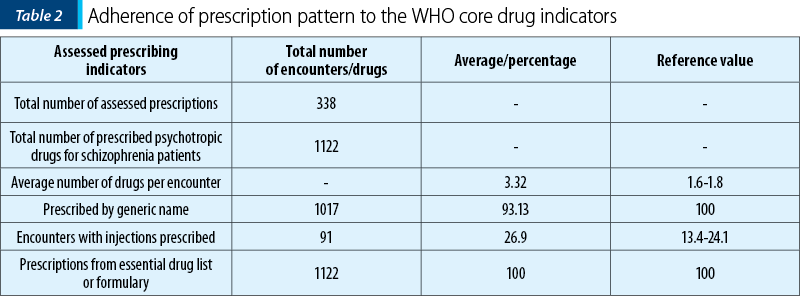
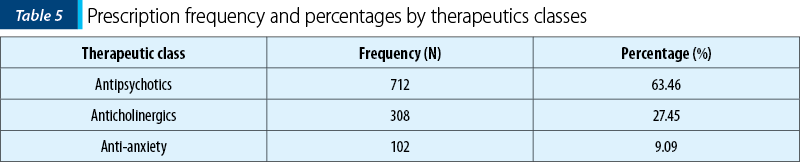
Out of total 698 encounters for patients with schizophrenia spectrum, 21 were excluded, the reason being incomplete prescription. However, 338 encounters were assessed after random sampling of every second prescription in 677 encounters. More male patients (176; 52.07%) were encountered in the prescriptions than females (162; 47.93%; Table 1), while the highest number of patients’ prescriptions were for those aged between 26 and 35 years old, with 63 males (48.09%) and 68 females (51.91%) – Table 1. There was a total of 1122 prescribed psychotropic medicines. However, the average number of prescriptions per encounter was 3.23 (Table 2). The maximum number per prescription was six drugs, while three drugs per prescription were mostly used (61.5%), and the least used was one drug per prescription (2.1%) – Table 6. Moreover, 95.97% of the total number of drugs were prescribed by generic names (Table 2), and in 26.9% of the total number of encounters, there were prescribed injections (Table 2). The antipsychotics were the most prescribed (63.46%), followed by anticholinergics (27.45%), while the least prescribed were anti-anxiety agents (9.09%) – Table 5.
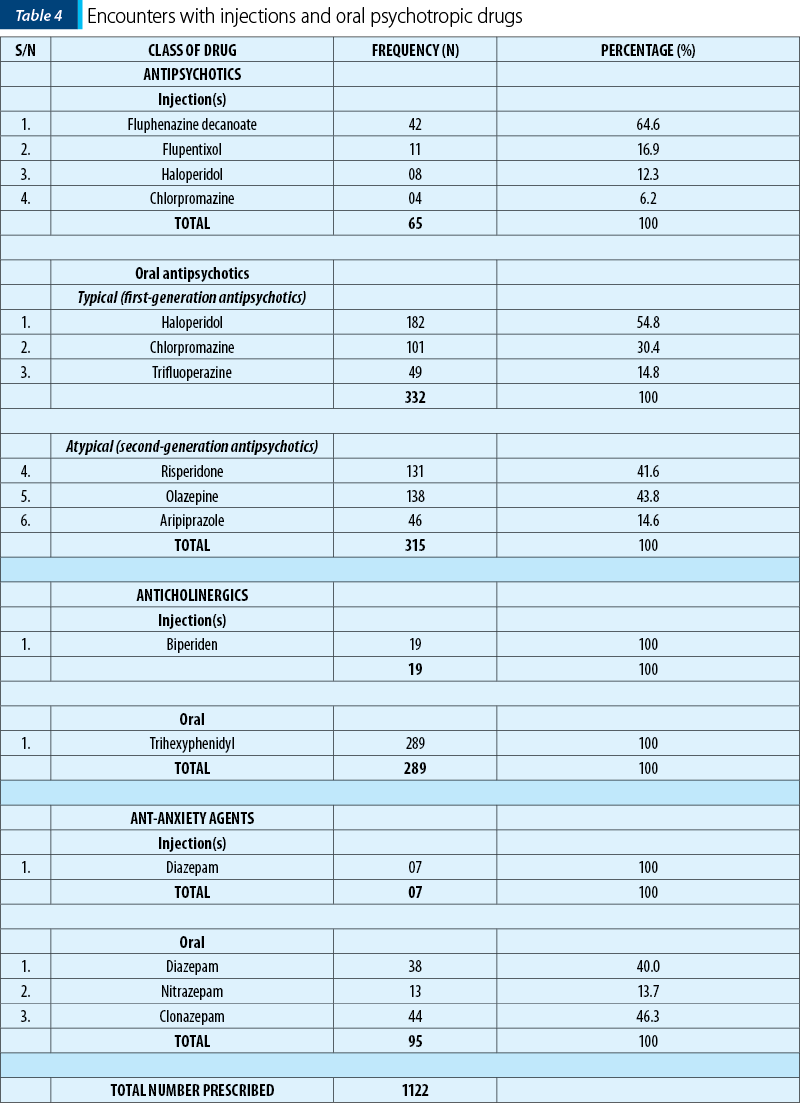
Out of the prescribed antipsychotic injections, fluphenazine was mostly used (42; 64.62%), while chlorpromazine was least prescribed (4; 6.15%) – Table 4. However, amongst all the psychotropic injections prescribed, fluphenazine remained the most prescribed (46.1%), followed by biperiden (20.9%), while the least used was chlorpromazine (4.4%) – Table 3.
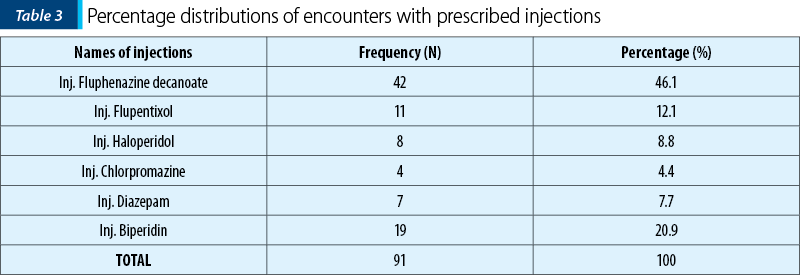
Among the oral antipsychotics, haloperidol (54.8%) and olanzapine (43.8%) were the most prescribed typical and atypical antipsychotics, respectively, while trifluoperazine (14.8%) and aripiprazole (14.6%) were the least prescribed typical and atypical antipsychotics, respectively (Table 4). However, biperiden and trihexyphenidyl were the only prescribed injectable and oral anticholinergics, respectively, while diazepam injection was the only prescribed injectable benzodiazepine (Table 3). Furthermore, the most prescribed oral benzodiazepine was clonazepam (46.3%), followed closely by diazepam (40%), while nitrazepam was the least prescribed (13.7%) – Table 4.
4. Discussion
Psychotropic medicines are essential in the management of schizophrenia. We found in our study that three classes of psychotropic drugs were used, and they include antipsychotics, anxiolytics, and anticholinergics. However, antipsychotics remain the mainstay which can be seen in the result where these drugs (oral and injections) accounted for 63.46%, out of the classes of psychotropics prescribed (Table 5). This result is similar to that of a study conducted in a South West Ethiopia on schizophrenia patients prescriptions(9).
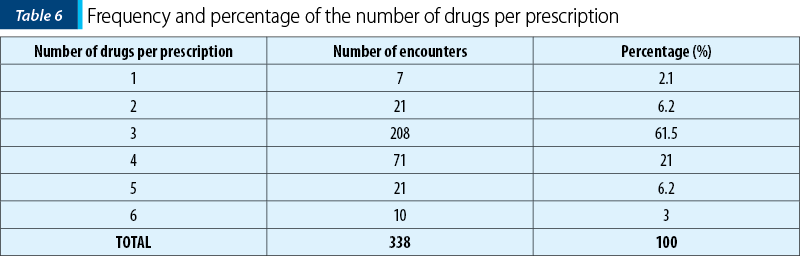
In psychiatry, polypharmacy can be defined as the use of two or more psychiatric medications in a patient(11), or the use of two or more medications that have the same pharmacological actions to treat the same condition(12). The reference value for the average number of drugs per encounter to assess polypharmacy is between 1.6 and 1.8, and in our study, we found that the value of the average number of drugs per encounter was 3.32, which is quite higher than the reference value (Table 2).
Trihexyphenidyl is an anticholinergic that reduces the side effects of antipsychotics, especially of the typical ones, which are associated with extrapyramidal effects. Our study shows that trihexyphenidyl is the only anticholinergic used, and the majority (27.45%) of the prescriptions contained this drug (Table 5.) Furthermore, the antipsychotic injections are mostly used in patients with schizophrenia to improve adherence and in patients with irregular contacts with outpatient psychiatric services(10). The reference value for WHO prescribing indicators for the use of injections is in the range of 13.4-24.1, but the results of our study revealed 26.9 (Table 2). We also found that fluphenazine decanoate accounted for 46.1% of the psychotropic injections (Table 3) and for 64.6% of the antipsychotics injections (Table 4), making it the most used psychotropic agent in our study. This formulation is less expensive and has a long-lasting effect, and this may be the reason for the result.
Less than 100% (93.3%) of the prescriptions were prescribed by generic names which is contrary to the WHO recommendation and reference value. The reason may be that some of the healthcare providers lack trust on the quality of some brands of psychotropic products. This result is similar to that of a study conducted in a tertiary hospital in Belagavi, India(13). Moreover, it was observed that all the psychotropic medicines used were in both the local and theWHO essential lists.
Conclusions
It was concluded that there were issues of polypharmacy, some reluctance in prescribing drugs with generic names, and overuse of injections.
Limitations of the study
Although the research was diligently performed, there were some limitations. Firstly, the prescribers were not approached to know the rationale for the prescriptions, and secondly, only one hospital was used. This does not reflect the prescriptions of other hospitals.
Recommendations
Further studies should be done in all the psychiatry hospitals in the country to know and compare the psychotropic medications prescription patterns for patients with schizophrenia. Furthermore, there is a need to create a structured way that will be consistent in knowing the medication adherence rate and quality of life of the patients.
Acknowledgement. Authors thank all the staff of the institution for their support. Special thanks go to Mrs. Ndukwe Charity for her willingness to assist and render information where necessary.
Corresponding author: Amala Chukwunwike Ofor E-mail: ofachcurepharm@gmail.com
CONFLICT OF INTEREST: none declared.
FINANCIAL SUPPORT: none declared.
This work is permanently accessible online free of charge and published under the CC-BY.

Bibliografie
-
Devora K. The State of Mental Health Globally in the wake of the COVID-19 Pandemic and Progress on WHO Special Initiative for Mental Health (2019-2023). World Mental Health Day. 10 October 2022. https://www.un.org/en/un-chronicle/state-mental-health-globally-wake-covid-19-pandemic-and-progress-who-special-initiative
-
Soroye MO, Oleribe OO, Taylor-Robinson SD. Community Psychiatry Care: An Urgent Need in Nigeria. J Multidiscip Healthc. 2021;14:1145-1148.
-
Schizophrenia. World Health Organization, 2022. https://www.who.int/net>Fact sheets>details
-
Laursen TM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annu Rev Clin Psychol. 2014;10:425-448.
-
Charlson F, Ommerem M, Flaxman A, Cornett J, Whiteford H, Saxena S. New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis. The Lancet. 2019;394(10194):240-248.
-
Kafle K. How to investigate drug use in health facilities. World Health Organization Report. WHO/DAP/93.1. 1993, pp. 1-87.
-
Krejcie R, Morgan D. Determining sample size for research activities. Education and Psychological Measurement. 1970;30(3):607-610.
-
Odusanya OO. Drug use indicators at a secondary health care facility in Lagos, Nigeria. Journal of Community Medicine and Primary Health Care. 2004;16(1):12-22.
-
Siraj J. Assessment of psychotropic medications prescribing pattern in Gebretsadik Shawo General Hospital, South West Ethiopia. Pan Afr Med J. 2023;45:165.
-
Barbui C, Bertolini F, Bartoli F, et al. Reasons for initiating long-acting antipsychotics in psychiatric practice: findings from the STAR Network Depot Study. Ther Adv Psychopharmacol. 2020;10:2045125320978102.
-
National Association of State Mental Health Program Directors: Technical Report on Psychiatry Polypharmacy. Medical Directors Council and State Medicaid Directors. Alexandria, Virginia: 2001.
-
Kukreja S, Kalra G, Shah N, Shrivastava A. Polypharmacy in psychiatry: a review. Mens Sana Monogr. 2013;11(1):82-99.
-
Mogali S, Kotinatot B. Drug utilization study of antipsychotics among schizophrenia patients in a tertiary care teaching hospital: a retrospective observational study. Int J Basic Clin Pharmacol. 2020;9(6):971-974.
Articole din ediţiile anterioare
Implicaţiile polimorfismelor genei MTHFR în etiologia schizofreniei
Studiul de față are ca scop identificarea mutațiilor în gena MTHFR, care pot reprezenta un factor de risc pentru apariția schizofreniei, participân...
Tulburările psihotice în ICD-11 comparativ cu ICD-10
Capitolul privitor la psihoze din ICD-11 prezintă modificări semnificative în raport cu ICD-10, începând cu plasarea în ordinea prezentării tulbură...
Delir religios la un pacient schizofren cu traseu EEG de tip iritativ în lobul temporal stâng
Schizofrenia este o tulburare psihiatrică ce este caracterizată prin simptome pozitive (delir şi halucinaţii), simptome negative (aplatizare afecti...
Implicaţiile traumei în dezvoltarea psihozei
Interesul asupra raporturilor dintre trauma din copilărie și adolescență și sănătatea mintală a crescut considerabil în ultimii ani. Este cunoscut ...