Two types of disasters – natural and, respectively, generated by humans – have been involved in psychiatric morbidity. Generally, the disasters generated by humans lead more frequently to persistent symptoms and psychiatric disorders. The severity of disaster agents and the degree of individual or population exposure to the disaster are considered predictors of psychiatric morbidity. Gender is a strong predictor of post-traumatic anxiety and depressive disorders. A second robust predictor of disaster mental health outcomes in individuals is represented by preexisting psychiatric disorders. Other but less consistent predictors of post-traumatic stress disorder (PTSD) after disasters include age, education and socioeconomic status. The disasters most frequently associated with detrimental consequences were those with an increased level of community destruction and those from developing countries with lower socioeconomic status. Supportive group interventions are recommended in the first days after the trauma. There is no consistent evidence regarding the effectiveness of early psychopharmacological approaches. Medication is recommended for symptoms’ improvement, especially in severe psychiatric symptoms that significantly impair functioning. Cognitive-behavioral short-term interventions in the first two weeks after trauma, focused on education, anxiety management training, imaginary and in vivo exposure therapy and in cognitive restructuring, proved the most effective.
Psihiatria dezastrelor
Psychiatry of disasters
First published: 30 noiembrie 2022
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Psih.71.4.2022.7329
Abstract
Rezumat
În morbiditatea psihiatrică au fost implicate două tipuri de dezastre: dezastrele naturale, respectiv dezastrele generate de om. În general, dezastrele provocate de om determină mai frecvent simptome şi tulburări psihiatrice persistente. Severitatea agenţilor cauzali ai dezastrelor şi gradul de expunere individuală şi populaţională la dezastru sunt consideraţi predictori ai morbidităţii psihiatrice. Sexul este un predictor puternic al tulburărilor de stres posttraumatic (PTSD), anxioase sau depresive. Al doilea predictor puternic este reprezentat de existenţa tulburărilor psihiatrice anterioare. Alţi predictori mai puţin relevanţi de PTSD şi psihopatologie postdezastre sunt vârsta, nivelul educaţional şi statutul socioeconomic. Dezastrele asociate cu consecinţe negative au fost cele cu un grad ridicat de distrugere a comunităţii şi din ţări în curs de dezvoltare cu un statut economic mai precar. În primele zile după traumă, sunt recomandate intervenţiile suportive de grup. Nu există dovezi consistente despre eficienţa intervenţiilor psihofarmacologice în fazele acute. Agenţii farmacologici sunt recomandaţi pentru ameliorarea în special a simptomelor psihiatrice intense care afectează semnificativ funcţionarea. Intervenţiile cognitiv-comportamentale pe termen scurt, efectuate în primele două săptămâni de la traumă, având ca obiective educaţia, antrenamentul pentru managementul anxietăţii, terapia de expunere imaginară, expunerea in vivo şi restructurarea cognitivă, s-au dovedit a fi cele mai eficiente.
Introduction
The World Health Organization (WHO) published in 2006 data regarding the natural disasters of 2005. Approximately 162 million people were affected worldwide by those disasters, 105,000 of them dying, and the total value of damages was over 176 billion USD(1).
Further assessments showed that the frequency of natural disasters related to weather conditions (hurricanes, tsunami) doubled in the past decade. Terrorism – such as World Trade Center attacks (2001), anthrax attacks in the US, the Madrid train explosion (2004), the London subway attack (2005) and repeated terrorist attacks in the Middle East – is responsible for a significant number of casualties. Moreover, the frequency of terrorist attacks has increased in the past years(2).
Wars are also responsible for an increased number of casualties and affected persons. According to WHO data, in the year 2000 there were 23 ongoing wars, involving more than 40 countries and a recorded number of over 300,000 deaths(3). The current war in Ukraine has generated an increasing number of casualties, although precise records are not available yet.
Public health measures, quarantine and restrictions involved by the influenza and, more recently, by the COVID-19 pandemic are also responsible for an increased number of persons affected, including deaths(4).
Terms and definitions
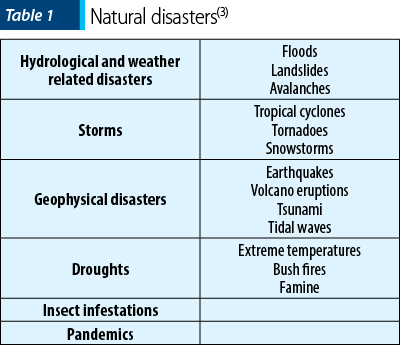
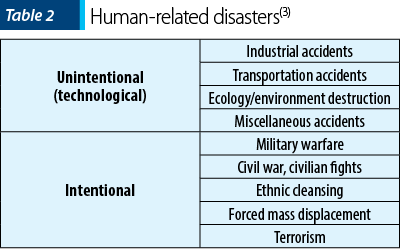
Disaster is defined as the result of the exposure to a danger characterized by threat to personal safety, community and family disruption. Henceforth, disasters generate major personal and social losses; moreover, they have multiple consequences that exceed the available existing resources. Literature describes two types of disasters: natural (Table 1) and human-generated (Table 2). Multiple studies show that human-generated disasters generate more frequently persisting psychiatric symptoms and disorders. The assessment of more than 60,000 victims of disasters who had significant impairment showed that 37% of them were exposed to mass violence, 29% to technological disasters, while 34% were exposed to natural disasters(3).
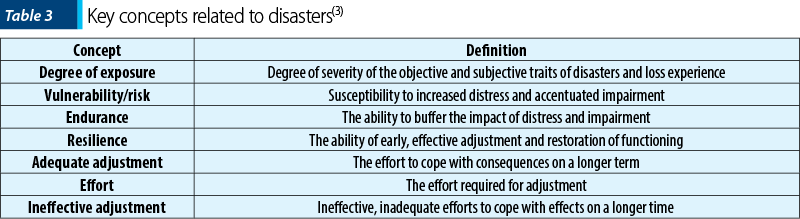
The key concepts regarding the impact of disasters are described in Table 3(3).
The severity of disaster agents and the degree of individual or population exposure to the disaster are considered predictors of post-traumatic stress disorder (PTSD). Gender is also a strong predictor of post-traumatic anxiety and depressive disorders. In the general population, compared to men, women exhibit twice the prevalence of PTSD, other anxiety disorders and major depression(6). A second robust predictor of disaster mental health outcomes in individuals is represented by preexisting psychiatic disorders(7). Other but less consistent predictors of PTSD after disasters include age, education and socioeconomic status(8).
Community response in disasters
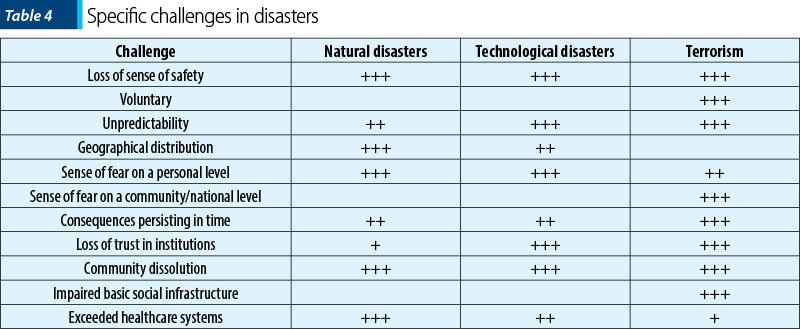
According to the impact of the disaster on the community, several specific challenges were identified. These challenges were estimated and evaluated for most disaster types. Loss of sense of safety, the voluntary and unpredictability features, geographic distribution, sense of fear/horror on a personal level, persisting consequences, loss of trust in institutions, community dissolution, and exceeded healthcare systems are among most cited (Table 4)(9).
Shortly after the disaster, there is a sense of cohesion and teamwork. With the passing of time, these are replaced by disillusionment and distrust. Consequently, rumors spread in the community regarding the context leading to the event and authority response, which in turn generate an increasing, persisting state of fear. A study of a school shooting in Illinois ascertained increased anxiety levels persisting one week after the event, even after the news that the assailant died by suicide. Subsequently, fear is replaced by anger, many times generated by the quest for the one responsible for the event, such as lack of preparation of the authorities and inappropriate authority response(10).
Neurobiological background of disaster psychiatry
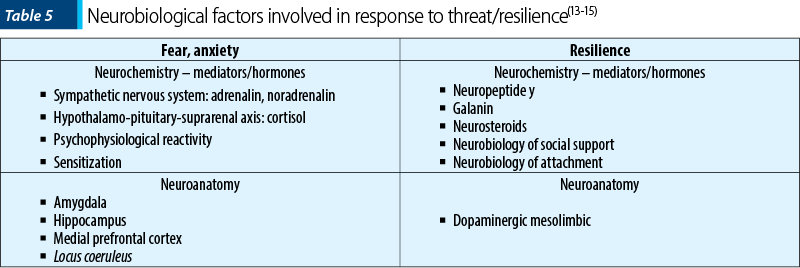
Multiple neurobiological systems are involved in the human response to threat. Simultaneous activation of various brain regions and neurotransmitter systems allows the organism to assess and respond to potential dangers. This dynamic process contributes to the development of anxiety, fear, and the “fight or flight” response(11).
Defense against danger is based on a complex process of recognition and appraisal of internal and external stimuli. Mainly, the prefrontal cortex regulates the strength and duration of this coping mechanism, and generally turns it off when it is appropriate to do so. The malfunction of regulatory systems, however, can lead to excessive fear, anxiety and significant impairment and disability in vulnerable individuals. Most neurobiological research in PTSD as well as in the neurobiology of resilience has been concentrated on two systems that are critical for survival: the sympathetic nervous system (SNS), and the hypothalamic-pituitary-adrenal (HPA) axis(11).
Findings from clinical physiological, receptor binding and pharmacologic studies have provided evidence for noradrenergic hyperreactivity in traumatized individuals with PTSD(11).
Most PTSD studies demonstrate alterations consistent with enhanced feedback inhibition of the HPA axis and increased HPA reactivity. The degree to which these abnormalities represent predisposing neurobiological risk factors for the development of PTSD versus consequences of trauma and/or living with PTSD is not yet clear(12).
Multiple evidences sustain that some neuroanatomic structures/regions are involved in the fear response. The most consistent data mention the amygdala and the hippocampus. There are also identified several key neural circuits and neurochemical systems that may underline human resilience in the face of uncontrollable stress(13-15).
Psychiatric morbidity
Multiple risk factors for psychiatric morbidity consecutive to disasters were identified. The most cited in literature are: consistent threat to life/survival, decreased predictability and controllability, relevant loss, probability of disaster repetition, direct exposure to physical injuries/death/dead bodies(16).
Psychiatric morbidity is influenced by the degree of impact of the disaster on the community, environment and on economy. Disasters associated with negative consequences were those with an increased degree of community destruction and those from developing countries with lower socioeconomic status. A study showed that loss of employment due to the disaster was a major negative predictor(17).
Terrorism differs from other natural or human-caused disasters through intense, persisting fear, decrease of trust in institutions, sense of loss of safety, and unpredictability(17,18).
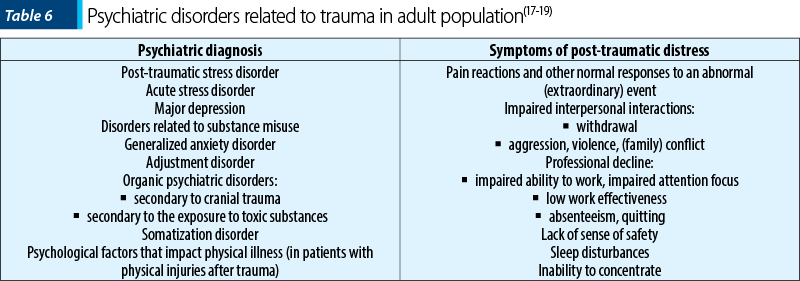
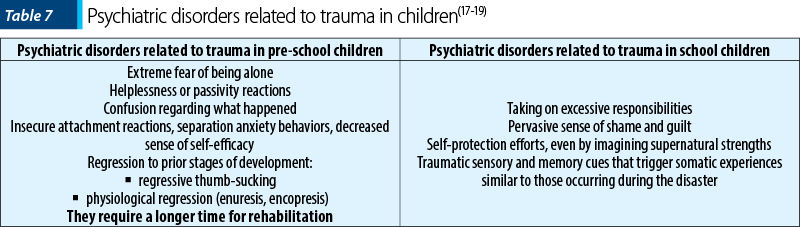
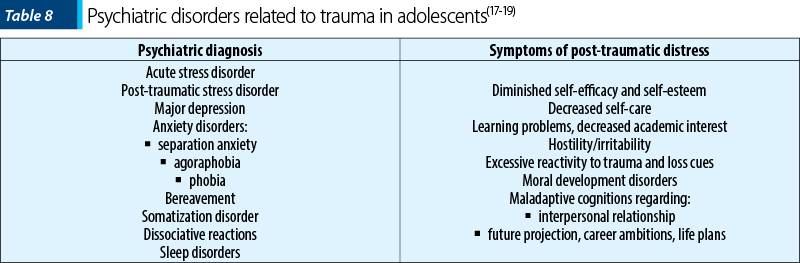
Epidemiological studies estimated the incidence of psychiatric disorders consecutive to disasters in various demographic groups (Table 6, Table 7, Table 8)(17-19).
Other studies tried to identify risk factors for psychiatric morbidity. The main factors thus identified were: direct exposure to life threats, injury, bereavement, single-parent families, children, seniors, women, preexisting PTSD, preexisting exposure to trauma, preexisting or current psychiatric disorder or physical illness, lack of supportive social/family relationships(17).
Moreover, studies identified factors that mediate or impair the recovery of children after disasters. Most studies mention: the frequency of exposure to trauma, loss, type and severity of stressors, quality of family functioning, unfavorable life circumstances (financial issues, overcrowding), school and community, quality of relationships with peers, physical injury, disability, co-occurring trauma and loss(19).
Effects of disasters on mental health entail psychiatric disorders and situations that generate distress, respectively. These should be differentiated, because each of the two requires distinct approaches. In persons without psychiatric disorders, directed interventions, such as disclosure of trauma to loved ones, may prove beneficial by increased social support and sharing. In psychiatric disorders, directed interventions and, in some cases, pharmacological therapy for a limited amount of time are necessary(8). Comorbid conditions should not be overlooked, because they often exist and are relevant for the course of rehabilitation and treatment selection. Based on current studies, acute onset and chronic PTSD are well known. The onset of psychiatric disorders is usually immediately after the disaster strikes, and their considerable chronic course may be anticipated. On the other hand, in some situations a diagnosis may not be established for many weeks after the disaster(19,20).
Phases of disasters and the role of mental health professionals
A multistage evolution of disasters was ascertained(21,22).
The heroic phase, corresponding to the first week of the disaster, elicits altruistic behaviors expressed in saving, providing shelter, food and support to peers. This phase is a preventive intervention for psychiatric disorders.
The “honeymoon” phase includes weeks 2-8, and the survivors are moved to safer places – support camps. Media attention, free of charge medical support, provision of free food and shelter are specific. Authority attitude is sympathetic, and free aid is provided by authorities. It also proves a preventive intervention for psychiatric disorders.
The disillusionment phase is the longest one: two to 36 months. Supplies, resources, media and authorities’ attention decrease. Survivors are confronted with the merciless work of post-disaster, and the prevalence of psychiatric morbidity requires treatment interventions.
Psychiatric consequences of disasters are influenced by the significance (cognitive appraisal) of the traumatic event, beliefs about the causes of disasters, and ramifications of these beliefs (such as self-blame, destructive inferences regarding human nature and anger towards the “responsible ones” when the event is assessed as preventable). Some events are more likely than others to generate loss of trust in an equitable, safe world(21).
Cognitive models of response to traumatic events indicate that their appraisal and the appraisal of their consequences are critical for stress levels and risk of post-event disorders. Catastrophic appraisals increase the experience of threat. Maladjustive appraisals are connected to beliefs that our world is unsafe, and to the sense of efficacy versus helplessness(22).
After disasters – especially after widespread incidents with acute psychopathology and anguish – mental health professionals are motivated by the need to help in the first hours and days. Nevertheless, the need for formal mental health services is higher in the following weeks and months, along with emerging psychiatric disorders in the affected population(22).
Services and clinical interventions in disaster psychiatry
Early intervention in disasters is essential in mitigating psychiatric morbidity. Early intervention must entail several factors: basic needs (food, shelter, medical services, information), immediate life threat/suicide risk, abilities, skills and impaired functioning(20).
In the early stages, several factors were identified which may affect recovery, such as: ongoing trauma, secondary stress factors (loss of resources), uncontrolled reactions, major risk factors (past trauma, bereavement, level of exposure), decreased resources (social support, adjustment skills, financial resources etc.), availability of information (TV, printed and online news, internet access, transportation). The person’s self-assessment focused on what they believe they need at the moment for recovery needs to be encouraged(20).
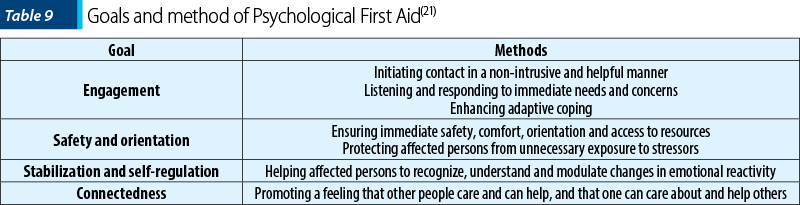
In the first 14 days after trauma, group supportive interventions are recommended(20,21). Psychological First Aid (PFA) main goals are the main factors that the early intervention strategies need to address – Table 9(21).
The Critical Incident Stress Debriefing (CISD) structured group intervention is constructed to explore facts, thoughts, reactions and coping strategies after trauma. Two randomized controlled trials of CISD reported a lower incidence of negative outcomes in those who received CISD compared with those who did not receive an intervention(23).
There is no consistent evidence of the effectiveness of pharmacological interventions in acute stages. Experts recommend pharmacological agents only for symptoms’ improvement, especially in intense psychiatric symptoms that significantly impair functioning(24,25).
Short-term cognitive behavioral interventions (4-5 sessions), aiming education, anxiety management training, imaginary exposure therapy, in vivo exposure and cognitive restructuring, proved the most effective and are always recommended in the first two weeks after trauma(26).
Special topics
The role of mental health service providers in disasters caused by the use of mass destruction weapons
Mass destruction weapons generating disasters are chemical agents, biological agents, radioactive materials and nuclear explosives. In case of disasters caused by weapons of mass destruction, the goals of mental health service providers are: consulting with other healthcare providers and planning the response strategy, development of triage protocol, identifying high-risk groups, and the treatment of psychiatric consequences. Community information and readiness, consultation with authorities, school system training, media education, counseling and training must also be included(27).
Planning of response to pandemics
In case of pandemics, interventions must address pre-pandemic preparedness, response to early stages of pandemic, response to advanced stages of the pandemic and recovery(28).
Recommended pre-pandemic preparedness includes: educating the population, authority training, information and readiness. In early stages of the pandemic, communication and information dissemination are essential; they are proven important first measures in an identified or suspected infectious outbreak with pandemic potential. In advances stages of the pandemic and in recovery stage, the proposed measures are represented by: support and reconstruction of community structure and functioning, ensuring necessary work resources, decrease of helplessness and renewed optimism. Virtual connectedness (web, phone, TV, radio) is crucial in these stages. Gathering places, such as religious centers, schools, postal offices and stores, may represent access points for education, instruction and distribution(28).
Exposure to traumatic deaths during disasters
In the context of exposure to traumatic deaths during disasters, the identified stressors are grouped chronologically: prior to exposure, during exposure, and after exposure(29).
Stressors identified prior to exposure (anticipatory) are: lack of information regarding tasks and roles, and anticipation of persons’ reaction to viewing traumatic deaths of other persons. Stressors during exposure (onsite) are: sensory overload, handling of personal belongings of victims, fatigue, excessive commitment, intense individual emotions and perceived individual threat. Stressors after the exposure (post-event) with increased traumatic potential are represented by the need for information and intense emotions (such as sadness or alienation)(29,30).
Bibliografie
-
Bulletin of the World Health Organization. 2006 Jan;84(1).
-
Rubin GJ, Brewin CR, Greenberg N, Simpson J, Wessely S. Psychological and behavioural reactions to the bombings in London on 7 July 2005: cross sectional survey of a representative sample of Londoners. BMJ. 2005;331(7517):606.
-
Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981-2001. Psychiatry. 2002;65(3):207-239.
-
Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord. 2020;277:55-64.
-
Compas BE, Connor-Smith JK, Saltzman H, Thomsen AH, Wadsworth ME. Coping with stress during childhood and adolescence: problems, progress, and potential in theory and research. Psychol Bull. 2001;127(1):87-127.
-
Breslau N. Gender differences in trauma and posttraumatic stress disorder.
-
J Gend Specif Med. 2002;5(1):34-40.
-
Liao SC, Lee MB, Lee YJ, Weng T, Shih FY, Ma MH. Association of psychological distress with psychological factors in rescue workers within two months after a major earthquake. J Formos Med Assoc. 2002;101(3):169-176.
-
North CS, Nixon SJ, Shariat S, et al. Psychiatric disorders among survivors of the Oklahoma City bombing. JAMA. 1999;282(8):755-762.
-
Ghodse H, Galea S. Tsunami: understanding mental health consequences and the unprecedented response. Int Rev Psychiatry. 2006;18(3):289-297.
-
Schwarz ED, Kowalski JM. Malignant memories: PTSD in children and adults after a school shooting. J Am Acad Child Adolesc Psychiatry. 1991;30(6):936-944.
-
Southwick SM, Friedman MJ. Neurobiological models of posttraumatic stress disorder. In The Mental Health Consequences of Torture, eds. E. Gerrity, T. M. Keane & F. Tuma, 2001, pp. 73–87. New York: Kluwer Academic/Plenum Publishers.
-
Yehuda R, Golier JA, Halligan SL, Meaney M, Bierer LM. The ACTH response to dexamethasone in PTSD. Am J Psychiatry. 2004;161(8):1397-1403.
-
Orr SP, Claiborn JM, Altman B, et al. Psychometric profile of posttraumatic stress disorder, anxious, and healthy Vietnam veterans: correlations with psychophysiologic responses. J Consult Clin Psychol. 1990;58(3):329-335.
-
Southwick SM, Bremner JD, Rasmusson A, Morgan CA 3rd, Arnsten A, Charney DS. Role of norepinephrine in the pathophysiology and treatment of posttraumatic stress disorder. Biol Psychiatry. 1999;46(9):1192-1204.
-
Smith MA, Davidson J, Ritchie JC, et al. The corticotropin-releasing hormone test in patients with posttraumatic stress disorder. Biol Psychiatry. 1989;26(4):349-355.
-
Wain HJ, Grammer GG, Stasinos J, DeBoer CM. Psychiatric intervention for medical and surgical patients following traumatic injuries. In: Ritchie EC, Watson PJ, Friedman MJ (eds.). Interventions Following Mass Violence and Disasters: Strategies for Mental Health Practice, 2006, pp. 278–299. New York: Guilford Press.
-
Makwana N. Disaster and its impact on mental health: A narrative review.
-
J Family Med Prim Care. 2019;8:3090-5
-
Math SB, Nirmala MC, Moirangthem S, Kumar NC. Disaster Management: Mental Health Perspective. Indian J Psychol Med. 2015;37(3):261-271.
-
Herrman H. Promoting Mental Health and Resilience after a Disaster. J Exp Clin Med. 2012;4(2):82e87.
-
Bryant RA. Psychosocial approaches to acute stress reactions. CNS Spectrums. 2005;10:116–122
-
Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims.
-
J Consult Clin Psychol. 2002;70(4):867-879.
-
Gray MJ, Maguen S, Litz BT. Acute psychological impact of disaster and large-scale tauma: limitations of traditional interventions and future practice recommendations. Prehosp Disaster Med. 2004;19(1):64-72.
-
McNally RJ, Bryant RA, Ehlers A. Does Early Psychological Intervention Promote Recovery From Posttraumatic Stress?. Psychol Sci Public Interest. 2003;4(2):45-79.
-
Watson P. Mental health interventions following mass violence. Stresspoints. 2004;12:4–5.
-
Watson PJ, Shalev AY. Assessment and treatment of adult acute responses to traumatic stress following mass traumatic events. CNS Spectrums. 2005;10:123–131.
-
Bryant RA, Moulds ML, Nixon RV. Cognitive behaviour therapy of acute stress disorder: a four-year follow-up. Behav Res Ther. 2003;41(4):489-494.
-
Shalev AY, Tuval R, Frenkiel-Fishman S, Hadar H, Eth S. Psychological responses to continuous terror: a study of two communities in Israel. Am J Psychiatry. 2006;163(4):667-673.
-
Ahmed QA, Arabi YM, Memish ZA. Health risks at the Hajj. Lancet. 2006;367(9515):1008-1015.
-
Ursano RJ, Fullerton CS, Kao TC, Bhartiya VR. Longitudinal assessment of posttraumatic stress disorder and depression after exposure to traumatic death. J Nerv Ment Dis. 1995;183(1):36-42.
-
Coenen P, van der Molen HF. What work-related exposures are associated with post-traumatic stress disorder? A systematic review with meta-analysis. BMJ Open. 2021;11(8):e049651.
Articole din ediţiile anterioare
Trauma psihică a expunerii la infecţia cu SARS-CoV-2
După mai mult de un an de expunere globală la COVID-19, la consecinţele acesteia asupra stării de sănătate şi la măsuri variabile de limitare a răs...
Aspecte de diagnostic şi tratament al tulburărilor asociate stresului profesional la personalul medical în contexul pand
Profesioniştii din domeniul sănătăţii se confruntă cu numeroşi factori de stres în practica de zi cu zi, iar datele existente în literatură arată o...
Tulburări psihice asociate traumatismului craniocerebral
Traumatismul craniocerebral necesită o abordare pluridisciplinară, în urma afectării din sfera neurologică şi psihiatrică, fiind o problemă majoră ...
Tulburarea de stres posttraumatic – provocări și priorităţi
Simptomele TSPT (reexperiențieri intruzive ale traumei, evitare, hiperreactivitate psihofiziologică, detașare și amorțire), indiferent de maniera î...